The Glasgow Coma Scale is a standardized assessment used to assess the level of consciousness in individuals who have suffered a severe TBI alone.
TBI Assessment
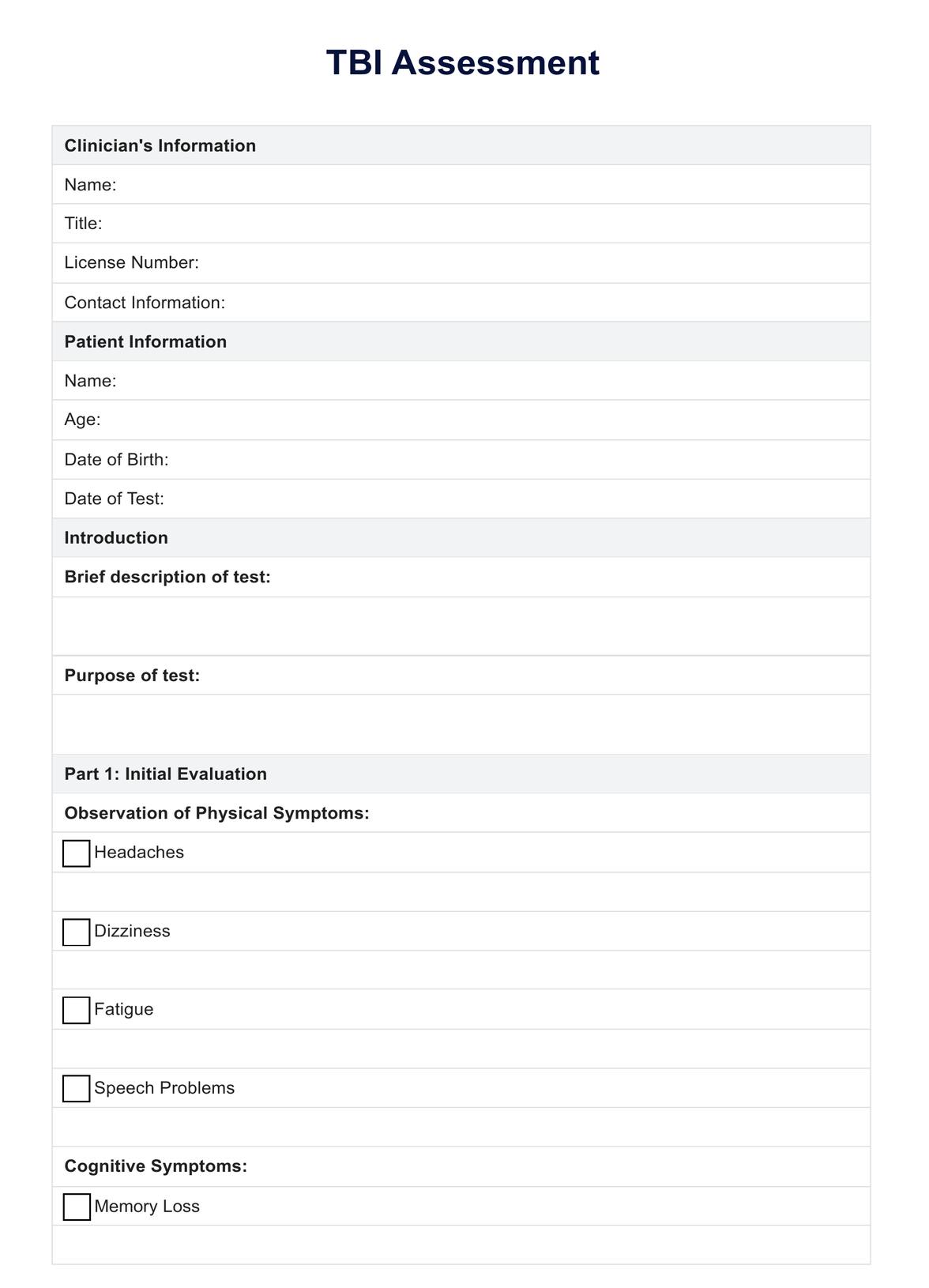
Explore our comprehensive guide on TBI Assessment, including a free downloadable example, benefits, and interpretation tips.
Use Template
TBI Assessment Template
Commonly asked questions
Even mild TBIs can have long-term cognitive and emotional effects, making early assessment and monitoring important.
Imaging tests like CT scans or MRIs are often used in TBI assessment, especially if the injury is suspected to be moderate or severe.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











