Medical professionals, especially neurologists and emergency room staff, use these scales to quickly assess and categorize stroke severity.
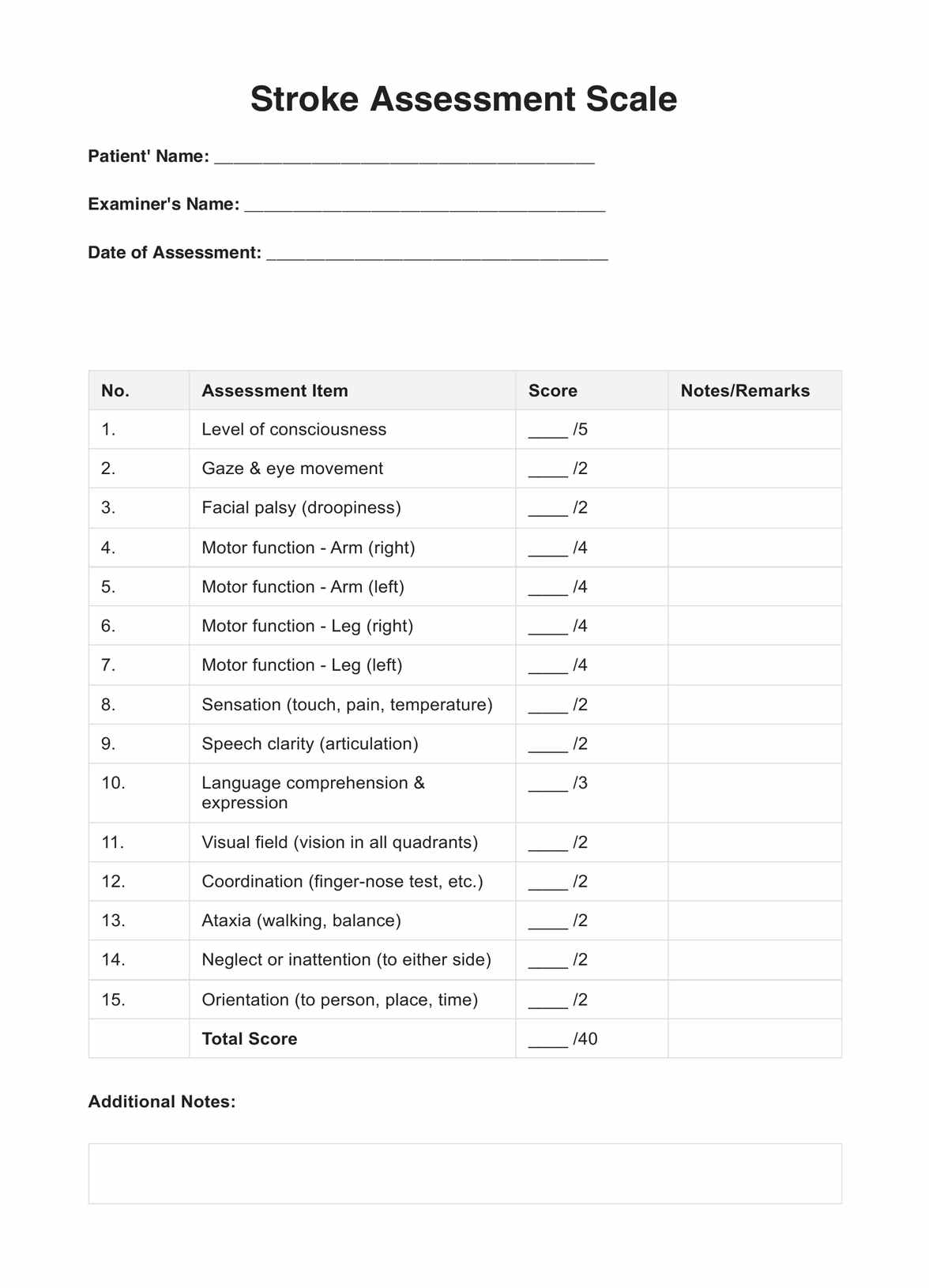
Stroke Assessment Scales
Discover the benefits and intricacies of the Stroke Assessment Scale with Carepatron—essential for timely and accurate evaluations in stroke patient care.
Use Template
Stroke Assessment Scales Template
Commonly asked questions
Primarily in the immediate aftermath of a suspected stroke, to guide treatment and predict outcomes.
You can use the scale through observing specific symptoms and assigning scores based on set criteria.. The summed scores then guide further action.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











