Common orthopedic exams include a range of motion tests, palpation, gait analysis, strength testing, and special tests like the McMurray Test for knee injuries and the Hawkins-Kennedy Test for shoulder impingement. These exams help diagnose conditions affecting the musculoskeletal system.
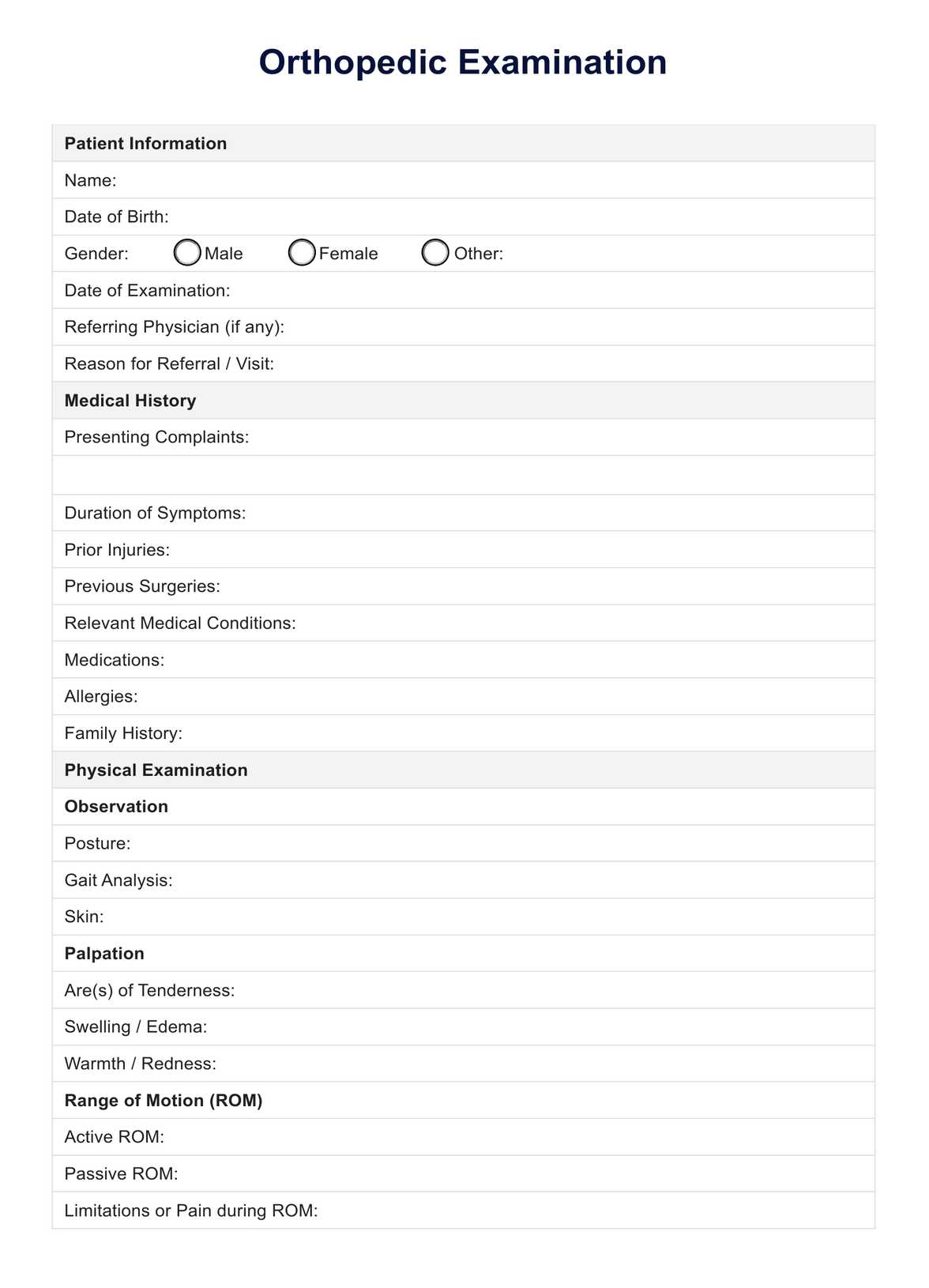
Orthopedic Examination
Explore the essentials of Orthopedic Examination with our comprehensive guide. Includes a detailed example and a free PDF download for healthcare professionals.
Orthopedic Examination Template
Commonly asked questions
A positive orthopedic test indicates the likelihood of a specific musculoskeletal condition being present. It means the test has elicited a response or finding, such as pain or abnormal movement, that supports the diagnosis of a particular injury or disorder.
Common orthopedic infections include osteomyelitis (infection of the bone), septic arthritis (infection in the joint), and bacterial tenosynovitis (infection of the tendon sheath). These infections can be caused by bacteria, such as Staphylococcus aureus, and require prompt medical treatment to prevent further complications.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











