What is a Normal Fetal Heart Rate Chart?
A Normal Fetal Heart Rate Chart is a graphical depiction of the normal range of fetal heart rates throughout pregnancy. It is crucial for caring for expectant mothers and their unborn children. Fetal heart rate, a vital indicator of cardiovascular health, exhibits dynamic changes as pregnancy progresses.
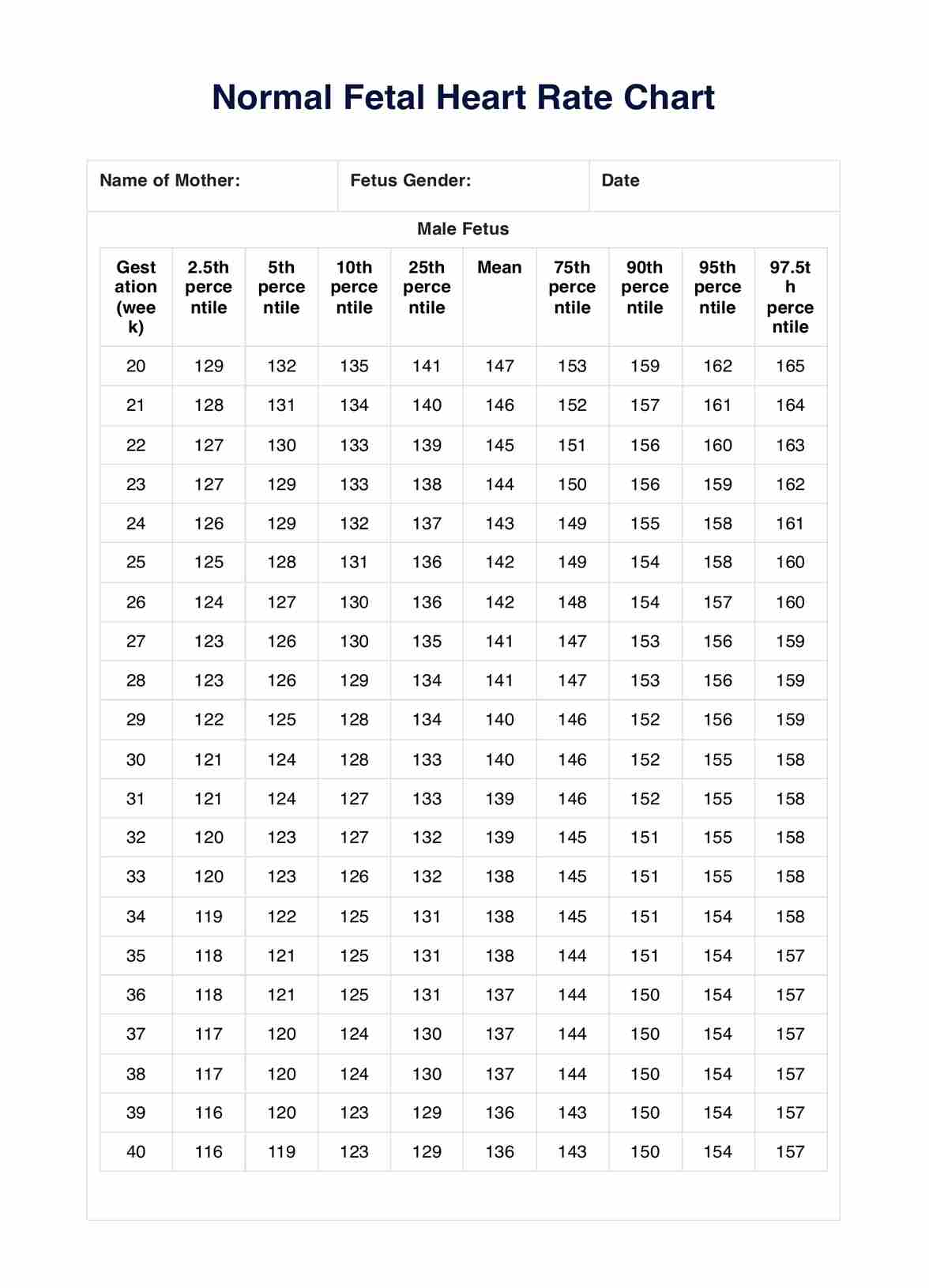
In the early stages, a normal fetal heart rate hovers around 110 beats per minute (BPM), gradually transitioning as the pregnancy advances. By the ninth week, the rate may increase to 140 to 170 BPM, underscoring the dynamic nature of fetal development. As pregnancy continues, the heart rate stabilizes, maintaining a typical range of 110 to 160 BPM.
Monitoring fetal heart rate is imperative, given its direct correlation with the overall well-being of the unborn child. The Normal Fetal Heart Rate Chart acts as a visual guide, facilitating healthcare professionals to interpret and understand the implications of deviations from the norm. Anomalies, such as an excessively high heart rate, may signal fetal distress or maternal fever, necessitating prompt investigation.
Conversely, a persistently low heart rate could indicate issues with fetal oxygenation, prompting a thorough exploration of potential causes.
The Normal Fetal Heart Rate Chart, coupled with the awareness of the normal heart rate ranges, equips healthcare providers with a comprehensive toolset to ensure timely interventions and optimal care for both mother and child. Boost your practice and improve client outcomes by exploring our heart rate chart template.