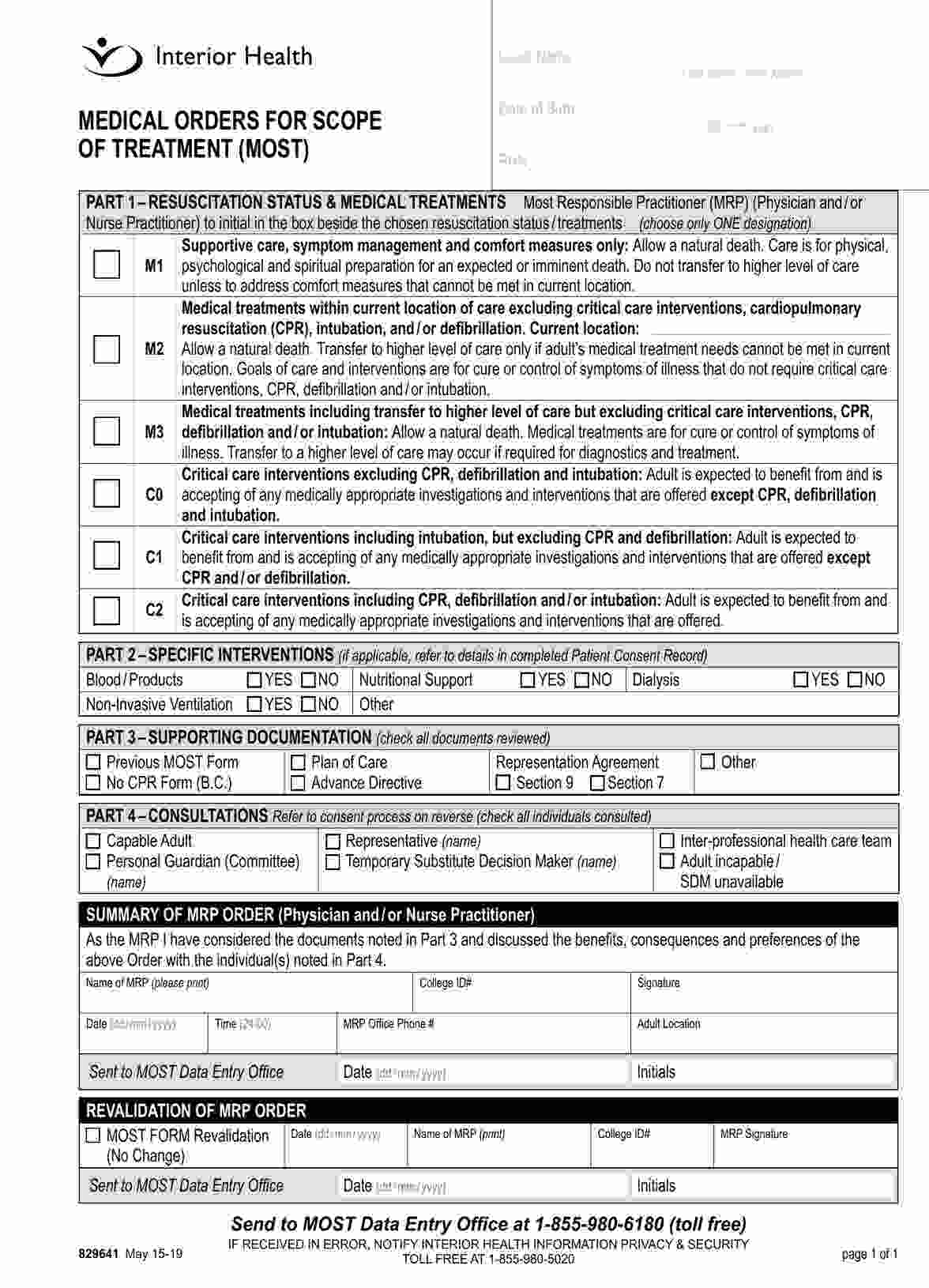
MOST, MOLST, POST, and POLST forms all aim to document patient preferences for end-of-life care but differ mainly in terminology and usage across various states or regions. They share similar goals but are named differently based on local adoption and legal frameworks.
MOST Medical Form
Discover the essential guide to the MOST Medical Form, including a comprehensive overview and a free PDF example. Ideal for healthcare professionals and users.
MOST Medical Form Template
Commonly asked questions
A DNR (Do Not Resuscitate) order specifically addresses the patient's wish not to receive CPR in case of cardiac or respiratory arrest. At the same time, a MOLST (Medical Orders for Life-Sustaining Treatment) covers a broader range of life-sustaining treatments beyond CPR, including patient preferences on intubation, ventilation, and more.
The MOST form is not universally required but is highly recommended for individuals with serious illnesses or those who want to ensure their treatment preferences are respected across healthcare settings. Its necessity varies based on patient needs and local regulations.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











