Doctors and sometimes patients request these tests when dealing with lung cancer, especially if they seek personalized treatment or have a family history of the disease.
Lung Cancer Genetic
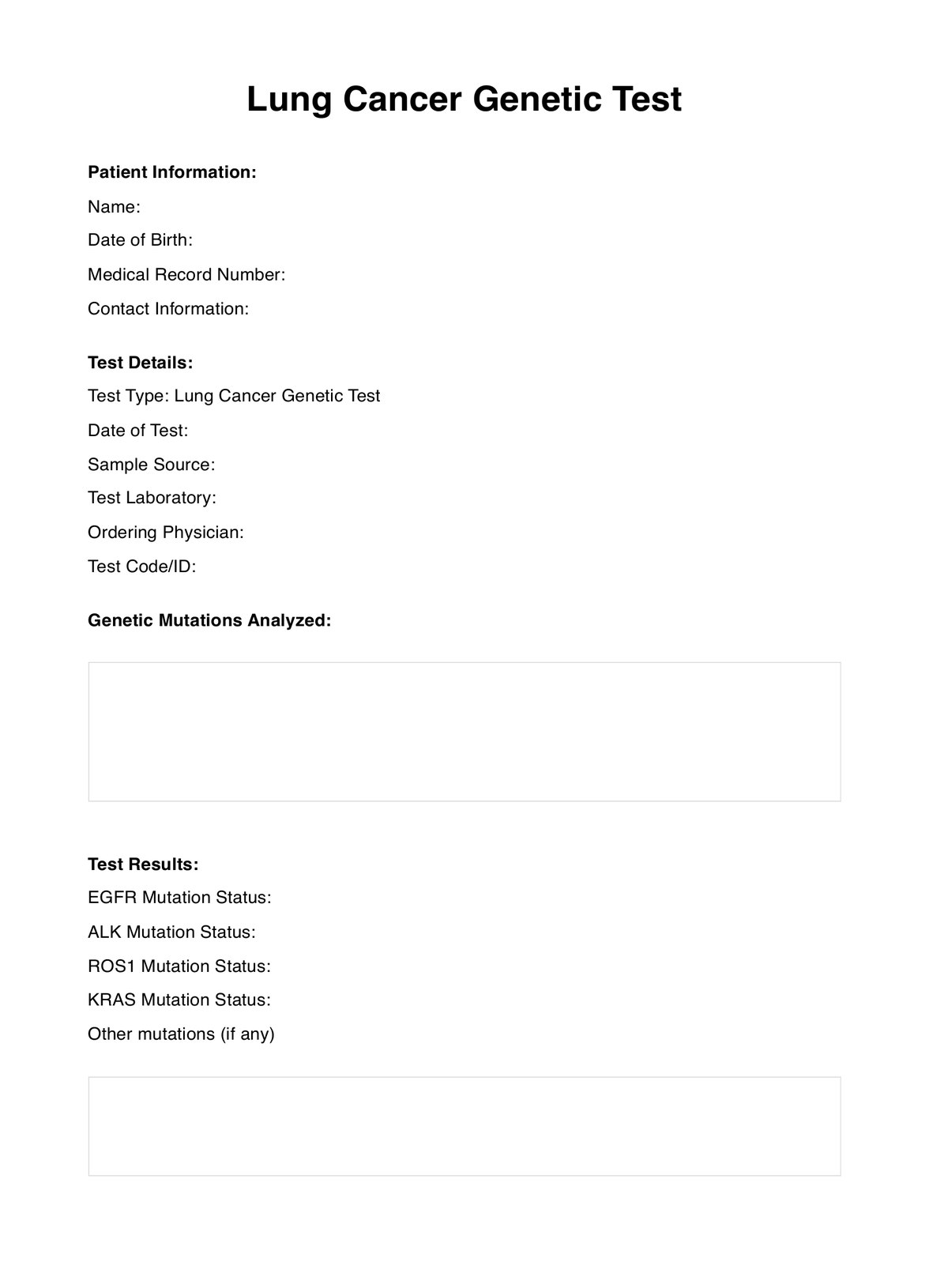
Offer advanced genetic insights to your patients with Lung Cancer Genetic Tests for healthcare professionals.
Use Template
Lung Cancer Genetic Template
Commonly asked questions
These tests are used during diagnosis to guide treatment choices and can be repeated during treatment changes or when exploring different therapies.
These tests analyze tumor samples to find specific gene mutations. The results help decide the best treatment, like targeted therapies matched to a patient's genes.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











