The OGTT (oral glucose tolerance testing) is the gold standard for diagnosing diabetes, as it is a blood glucose measurement and measures fasting glucose test the body's ability to use glucose effectively.
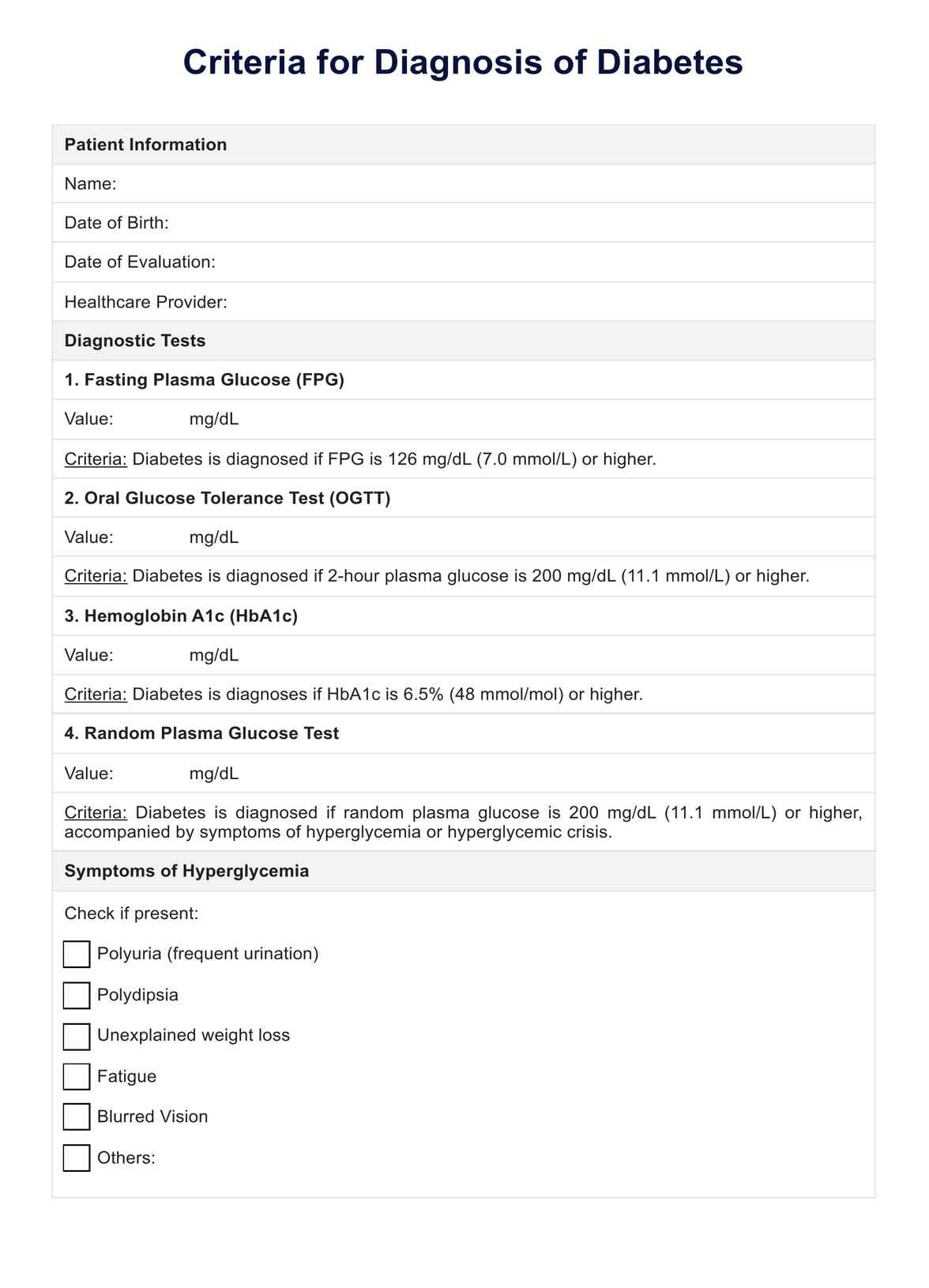
Criteria for Diagnosis of Diabetes
Streamline diabetes management with Carepatron's templates for accurate diagnosis, early treatment, care plans, and effective patient strategies.
Use Template
Criteria for Diagnosis of Diabetes Template
Commonly asked questions
The ADA recognizes several criteria, including fasting plasma glucose levels of 126 mg/dL or higher, A1C levels of 6.5% or higher, and plasma glucose levels of 200 mg/dL or higher during an OGTT.
The four primary tests are the fasting plasma glucose test, the OGTT, the A1C test, and random plasma blood glucose during the glucose testing.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











