Healthcare practitioners, such as doctors and pharmacists, typically request Therapeutic Drug Monitoring (TDM) for patients who are on medications that require close monitoring, such as those with a narrow therapeutic range or complex dosing regimens.
Therapeutic Drug Monitoring
Optimize patient care with Therapeutic Drug Monitoring. Ensure medication effectiveness and safety. Learn more.
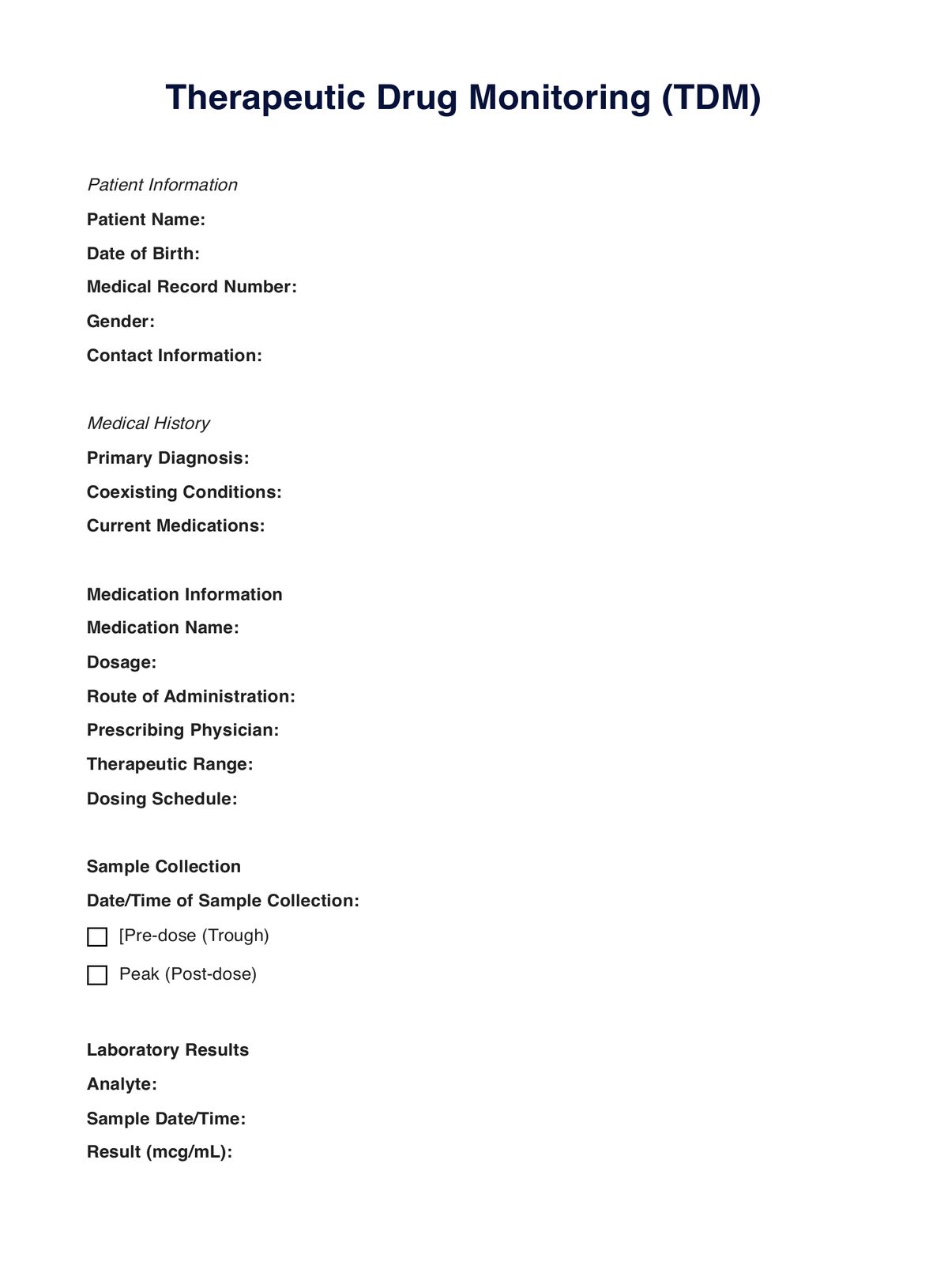
Therapeutic Drug Monitoring Template
Commonly asked questions
TDM is used when optimizing medication dosages is essential. It's employed when managing medications with a narrow therapeutic range, ensuring patient safety, and personalizing treatment regimens to individual needs.
TDM involves regular measurements of drug concentrations in a patient's bodily fluids, typically blood. These measurements guide healthcare practitioners in adjusting medication dosages to maintain therapeutic levels, improve efficacy, and minimize potential side effects.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











