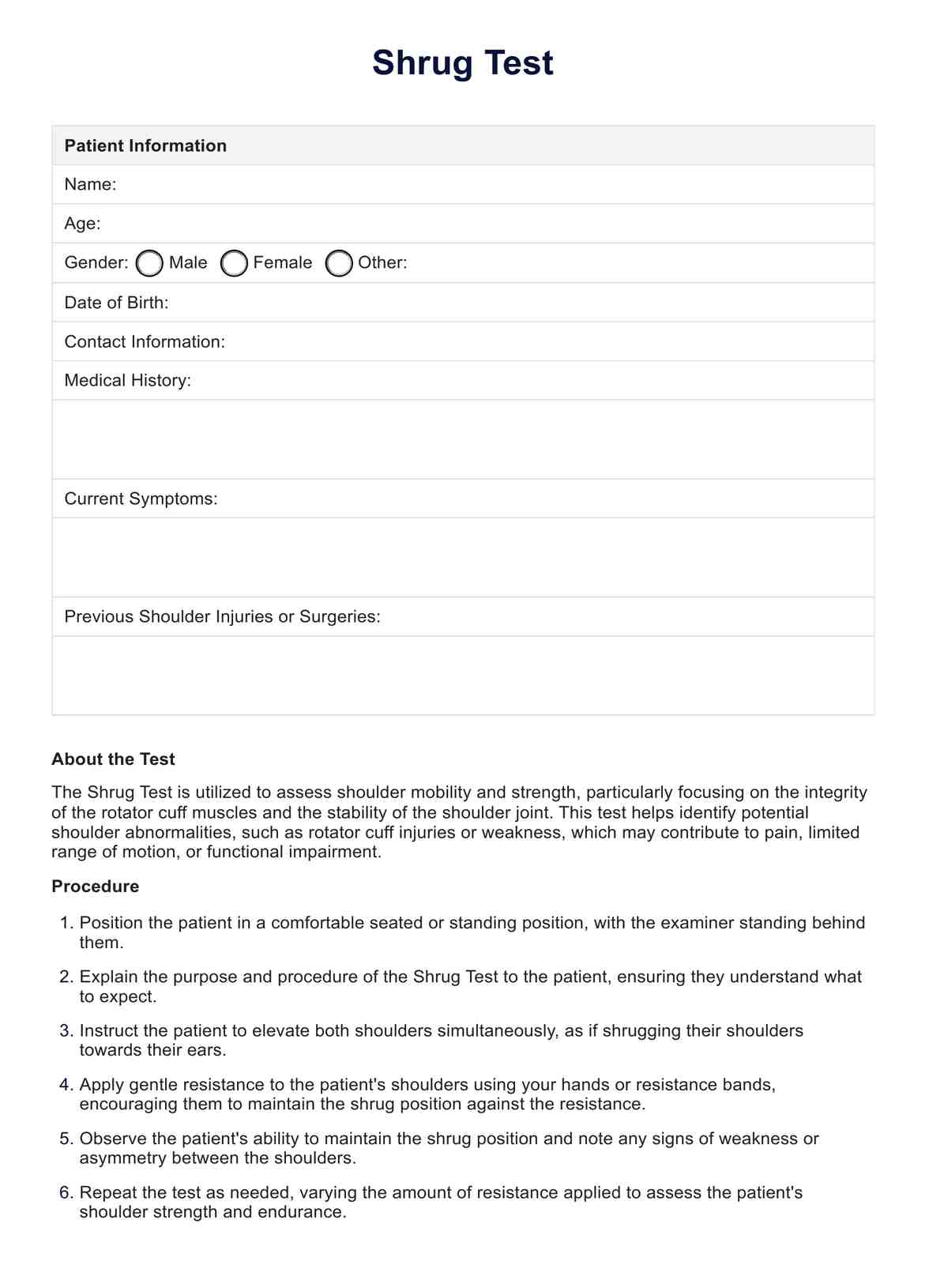
The Shrug Test is performed to identify potential shoulder abnormalities, such as rotator cuff injuries or weakness, which may contribute to pain, limited range of motion, or functional impairment. It helps clinicians diagnose shoulder conditions and guide appropriate treatment interventions.
Shrug Test
Evaluate shoulder mobility effectively with the Shrug Test. Assess range of motion for comprehensive healthcare diagnostics.
Shrug Test Template
Commonly asked questions
During the Shrug Test, the patient is instructed to elevate both shoulders simultaneously as if shrugging their shoulders towards their ears. The examiner applies resistance to the shoulders using their hands or resistance bands, and observes the patient's ability to maintain the shrug position.
A positive Shrug Test may indicate weakness or dysfunction in the rotator cuff muscles or the shoulder joint. Difficulty or asymmetry in maintaining the shrug position against resistance suggests underlying shoulder pathology, such as rotator cuff tears or adhesive capsulitis.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











