A Nursing Ear Assessment is a thorough evaluation of the external ear canal, middle ear, and inner ear to identify any abnormalities or signs of ear disorders. It typically entails a physical inspection, otoscopy (to look at the ear canal and tympanic membrane), hearing tests (to detect hearing impairment), and patient interviews (to understand symptoms like ear pain or discharge). Nurses also assess the need for interventions such as ear drops or hearing aids based on the patient's status.
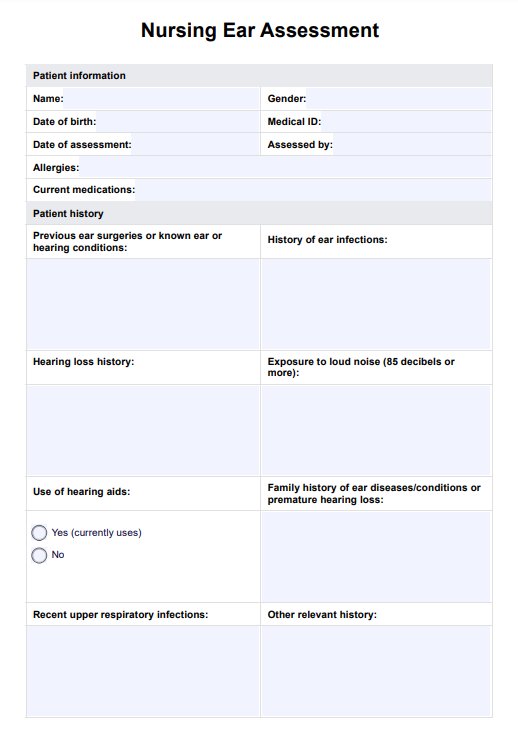
Nursing Ear Assessment
Guide to Nursing Ear Assessment: Covering patient history, pain, inspection, palpation, otoscopy, and essential hearing tests for healthcare professionals.
Nursing Ear Assessment Template
Commonly asked questions
Nurses perform basic hearing assessments to detect hearing impairment, including whispered voice tests and tuning fork tests. These determine if the patient has difficulty hearing, which might indicate issues within the external, middle, or inner ear. The nurse evaluates how the patient responds to auditory cues.
In pediatric ear assessments, nurses look for signs of frequent ear infections and middle ear fluid. They also check developmental milestones related to hearing and speech are being met. The prevalence of specific inner ear abnormalities and the approach to ear examination may differ from children to adults. Pediatric assessments often include observing behavioral cues and relying on reports from caregivers or teachers about the child's hearing and response to auditory stimuli.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











