Yes, care plans for impaired memory, based on the nursing diagnosis of impaired cognition, are designed to be flexible and can be adjusted as the individual's cognitive function changes. Regular evaluations, a crucial part of nursing interventions, allow healthcare professionals to update the plan to ensure it meets the current needs of those with Alzheimer's disease or other forms of cognitive impairment.
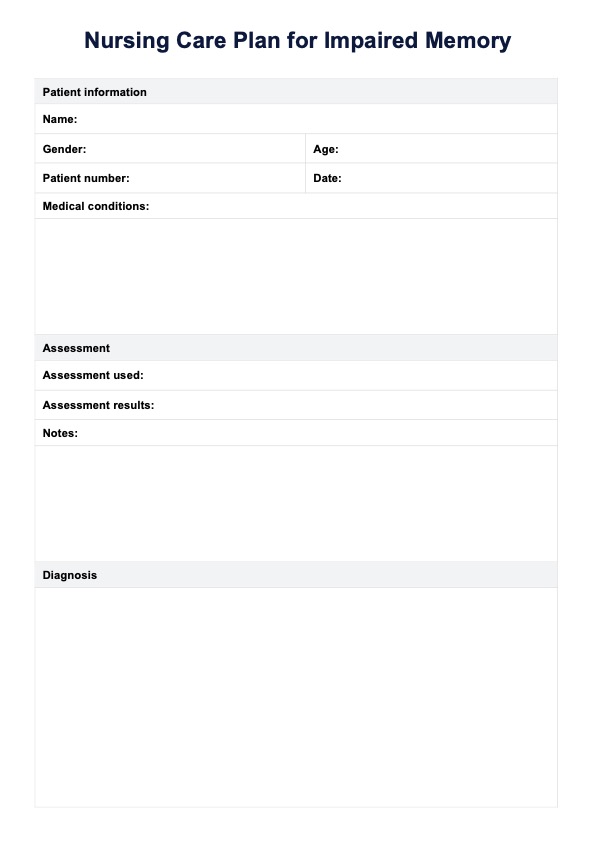
Nursing Care Plan for Impaired Memory
Discover our Nursing Care Plan for Impaired Memory to streamline your clinical documentation. Download a free PDF template here.
Nursing Care Plan for Impaired Memory Template
Commonly asked questions
Even in cases of mild memory impairment, a care plan can provide structure and strategies, such as creating a calm and structured environment, to help manage forgetfulness, maintain independence, and prevent cognitive decline. Early nursing interventions and supportive measures can significantly impact long-term outcomes for those experiencing the early stages of a progressive neurological disorder.
Creating a care plan for someone with impaired memory should involve a multidisciplinary team of healthcare professionals, including those with expertise in managing behavioral and psychological symptoms of dementia. This team should use their clinical judgment to address the nursing diagnosis and plan expected outcomes. The process should also involve individuals with cognitive impairment, their family members—who provide essential emotional support—and caregivers.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











