Chronic stress can significantly worsen osteoarthritis symptoms, intensifying pain and diminishing physical functionality. Effective stress management techniques are crucial for enhancing individuals' overall well-being and life quality with OA.
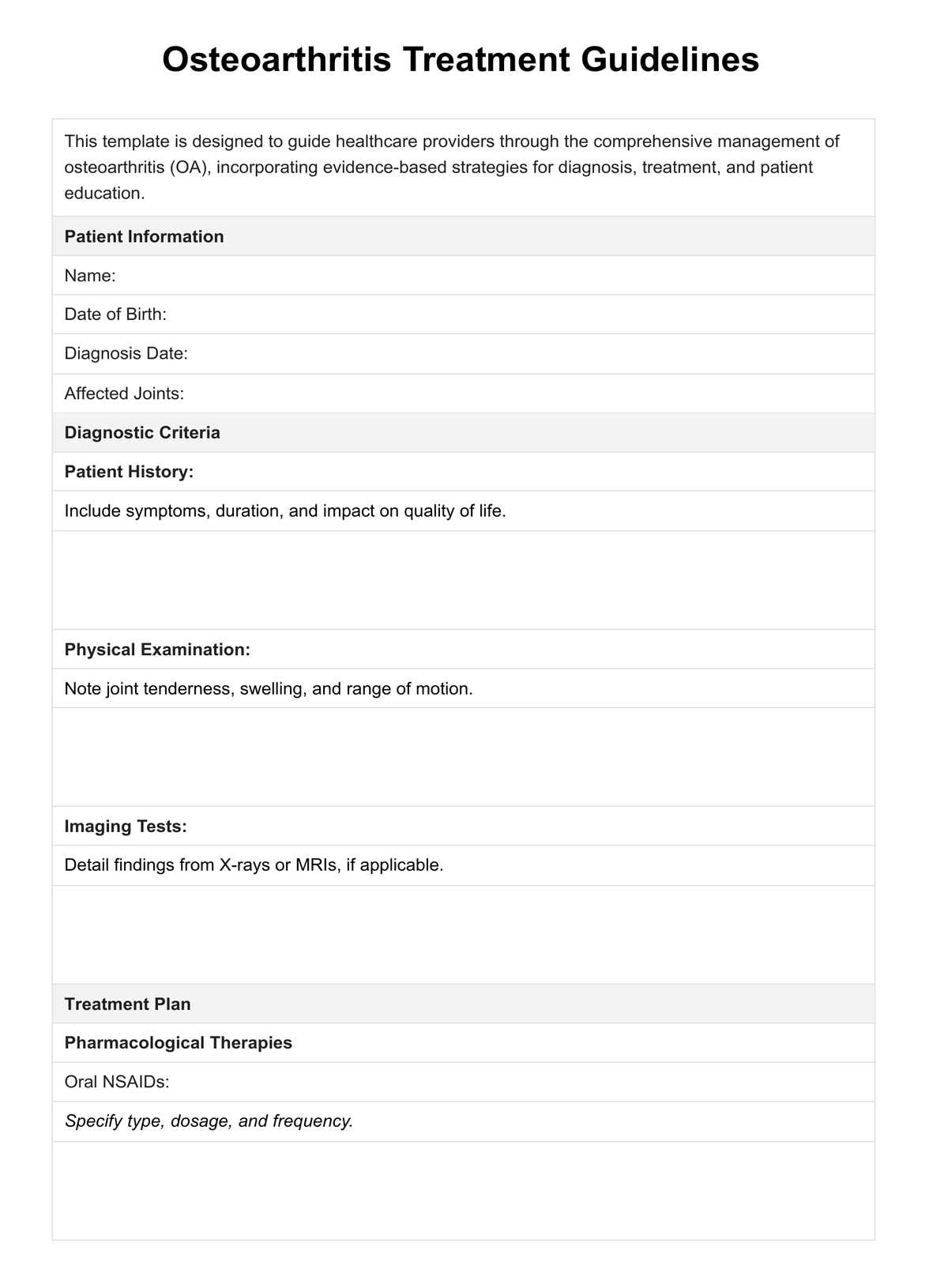
Osteoarthritis Treatment Guidelines
Learn about the management of osteoarthritis, treatments, causes, and care strategies. Access tips for managing symptoms and improving quality of life in our guide.
Osteoarthritis Treatment Guidelines Template
Commonly asked questions
A nutritious diet can play a pivotal role in managing osteoarthritis. Anti-inflammatory foods like fruits, vegetables, and omega-3-rich fish can help reduce joint inflammation and improve pain. Maintaining a healthy weight also reduces stress on the joints, alleviating symptoms.
While excessive or improper exercise can strain the joints, regular, moderate activity benefits OA patients. It strengthens the muscles around the joints, increases flexibility, and can help reduce pain and stiffness. Choosing low-impact exercises and consulting a healthcare provider for a personalized exercise plan is important.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











