A Nerve Conduction Test is a diagnostic procedure that measures the speed and strength of electrical signals traveling along nerves to evaluate nerve function and identify potential nerve damage or disorders of sensory nerves.
Nerve Conduction Test
Discover how Nerve Conduction Tests assess nerve function, aiding diagnosis & treatment planning. Learn more in our insightful overview.
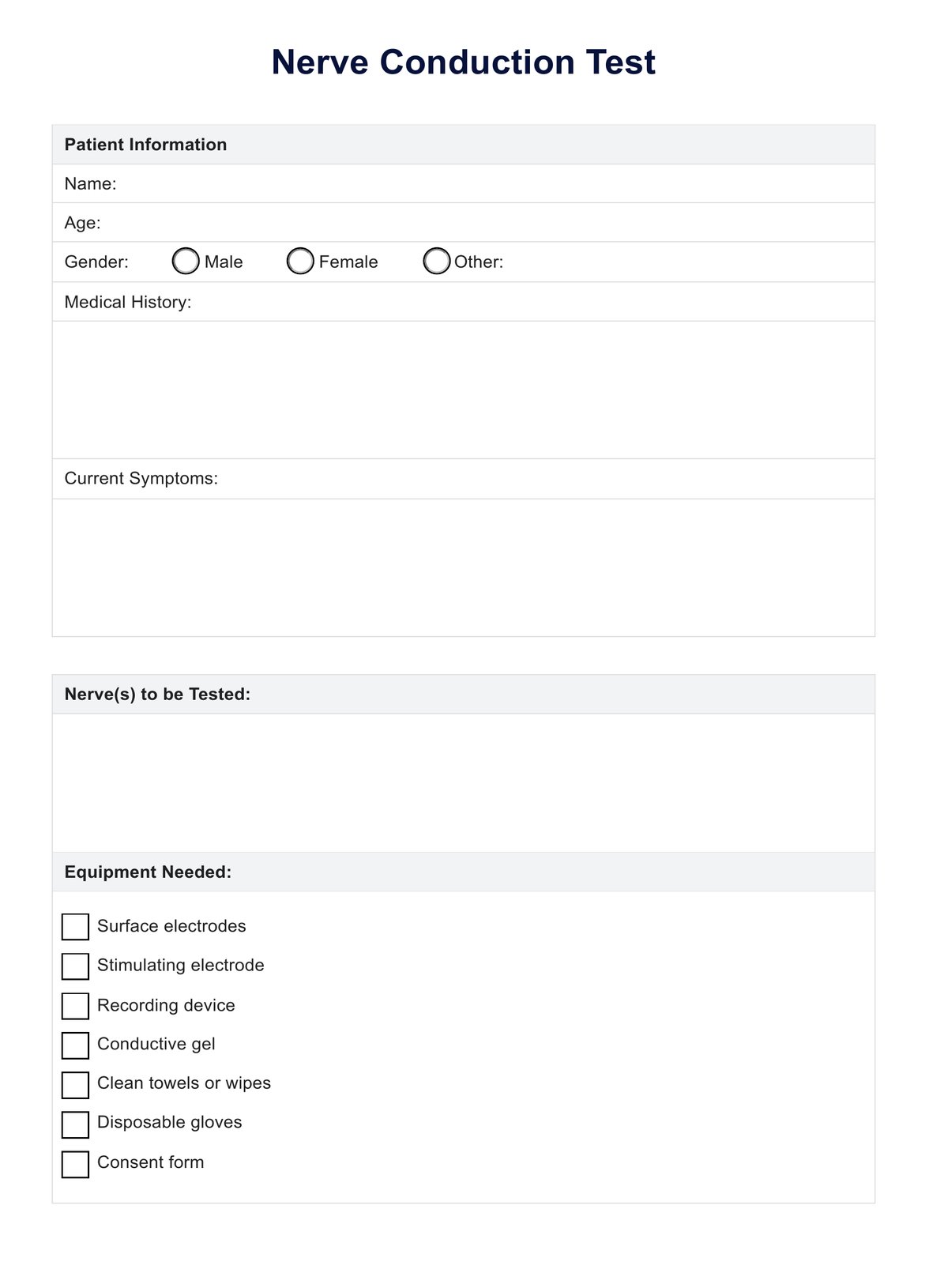
Nerve Conduction Test Template
Commonly asked questions
A Nerve Conduction Test may cause mild discomfort, such as a tingling sensation or mild muscle soreness, similar to what one might feel during electrical stimulation. However, it is generally well tolerated and not considered highly painful.
Yes, Nerve Conduction Tests are worth it as they provide valuable information about nerve health and function, aiding in accurately diagnosing and managing various neurological conditions, including carpal tunnel syndrome, peripheral neuropathy, and nerve injuries.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











