Medication reconciliation refers to the process of making the most accurate possible list of medications for a patient. This process involves verifying the patient's current medications, clarifying that the medications, doses, and frequency of the medications to be taken are appropriate, and reconciling the final list of medications for the patient.
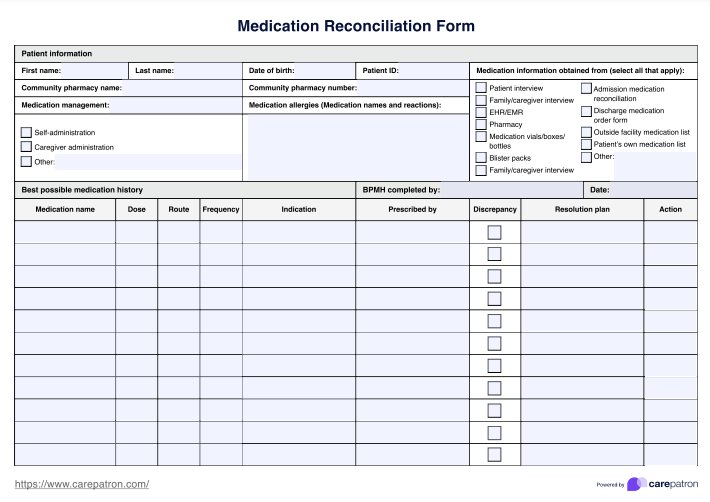
Medication Reconciliation Form
Ensure 100% accuracy of your patient’s medication list by using our detailed medication reconciliation form with separate best possible medication history.
Medication Reconciliation Form Template
Commonly asked questions
Some patients may have incomplete or conflicting medication histories due to transcription errors or missing information upon intake or transfer between institutions. Accurate knowledge of a patient's current medications is an integral part of every medical treatment or procedure, so it is worth investing time in reconciling a patient's medications if they have transitioned across services.
There is only so much you can do to obtain past medication information on your patient. If the records have been lost, deleted, or were not taken accurately in the first place, you cannot track them down. As such, we call it the best possible medical history, as you will create the best medication history from the information you have.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











