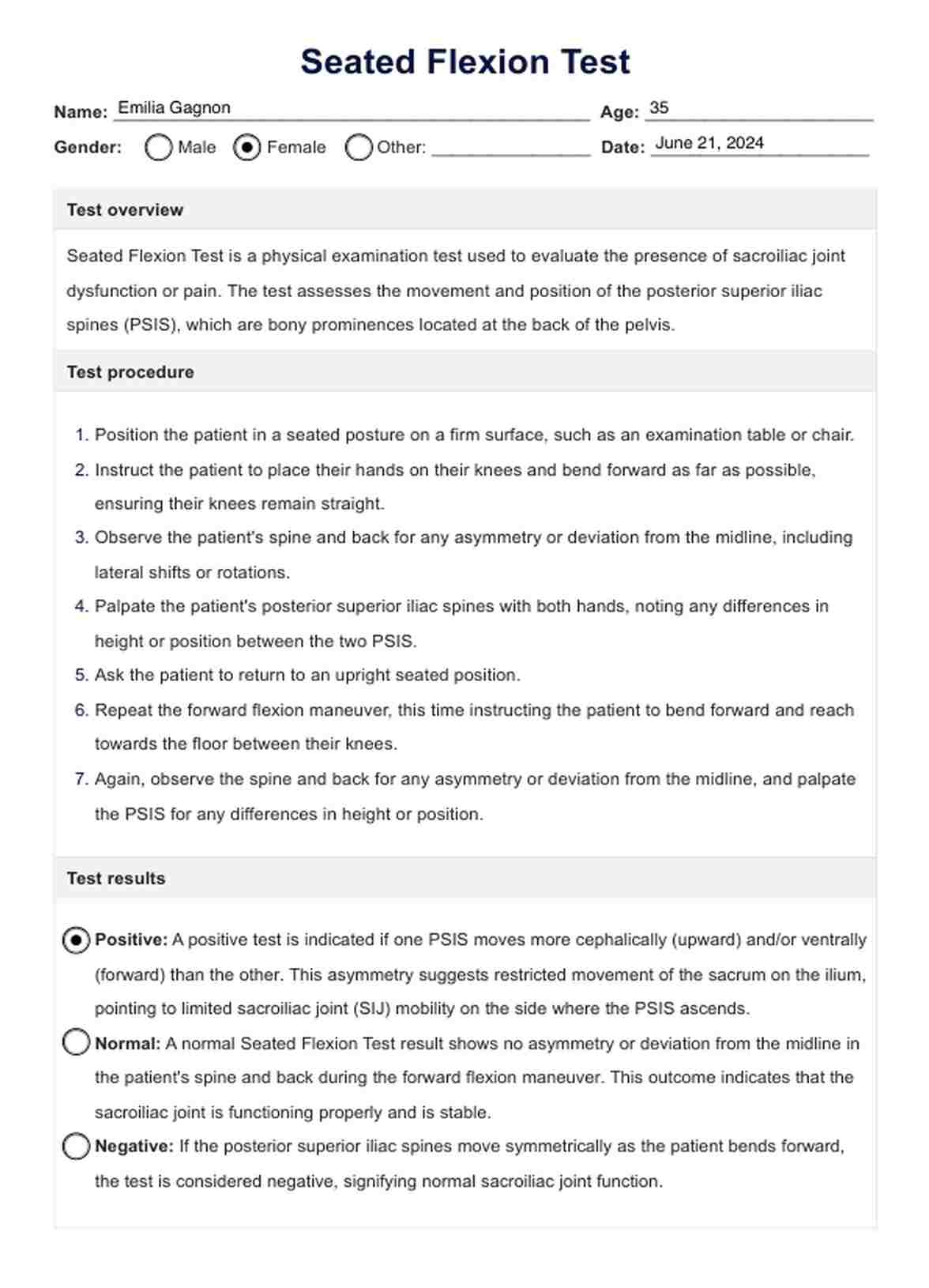
The seated flexion test is a diagnostic technique used to assess sacroiliac joint dysfunction by observing asymmetry in the movement of the posterior superior iliac spines (PSIS) when a patient bends forward from a seated position.
Seated Flexion Test
Learn all about the Seated Flexion Test with Carepatron's example and free PDF download. This comprehensive guide will help you understand the test and its applications.
Seated Flexion Test Template
Commonly asked questions
A positive standing flexion test indicates asymmetry or restriction in the motion of the sacroiliac joints when the patient bends forward from a standing position, suggesting dysfunction or imbalance in the pelvis or sacrum.
When performing a Seated Flexion Test, the examiner places their thumbs on the posterior superior iliac spines (PSIS) to palpate and monitor the movement of these bony prominences during the patient's forward bending motion.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











