A practical example of using the SBAR (Situation, Background, Assessment, Recommendation) communication tool would be a nurse calling a physician about a patient with sudden vital sign changes. An example situation would be: "I'm calling about Mr. Jones in room 305; his heart rate just jumped from 80 to 140 bpm." The background would cover: "He is two days post-op from a hip replacement and has a history of atrial fibrillation, but has been stable." Assessment involves the nurse's clinical judgment: "I believe he is experiencing a new onset of A-fib, his blood pressure is dropping slightly, and he is reporting dizziness." Finally, the recommendation is the requested action: "I recommend ordering an EKG stat and a dose of diltiazem per protocol, or would you like to come and assess him?"
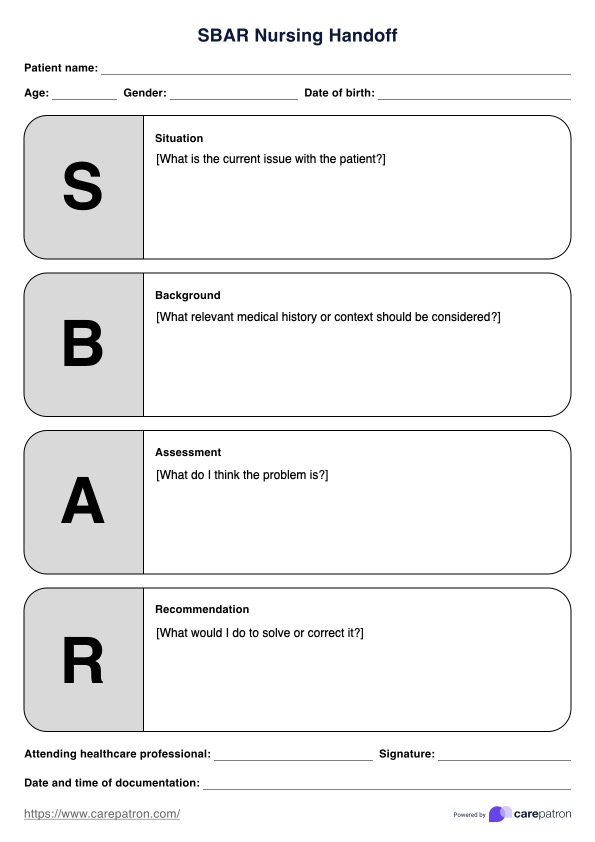
SBAR Nursing Handoff Template
Ensure continuity of care and patient safety by using an SBAR Nursing Handoff Template.
SBAR Nursing Handoff Template Template
Commonly asked questions
The 5 P's of Handoff are a mnemonic used to structure and ensure the completeness of patient information during a nursing shift change or transfer, guaranteeing all critical aspects are addressed for safe care continuity. The five components are: Patient (name, age, diagnosis, current status), Plan (the care plan, treatment goals, and pending orders), Purpose (the underlying rationale for the patient's treatment and interventions), Problems (current and potential issues, risks, or complications), and Precautions (any necessary safety measures, such as fall risk, allergies, or isolation).
To give an effective handoff report, the nurse should use a standardized communication structure, such as SBAR or the 5 P's, to ensure all critical and current information is transferred accurately and concisely. Begin by introducing the patient (Situation), summarizing the relevant medical Background and hospital course, detailing the current Assessment (including head-to-toe findings, vital signs, and recent labs), and offering specific Recommendations for the oncoming shift, prioritizing tasks and highlighting any critical changes or anticipated problems.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











