The three hallmark signs of Parkinson's disease are tremor at rest, bradykinesia (slowness of movement), and rigidity (muscle stiffness). These symptoms are key indicators used in diagnosing the condition.
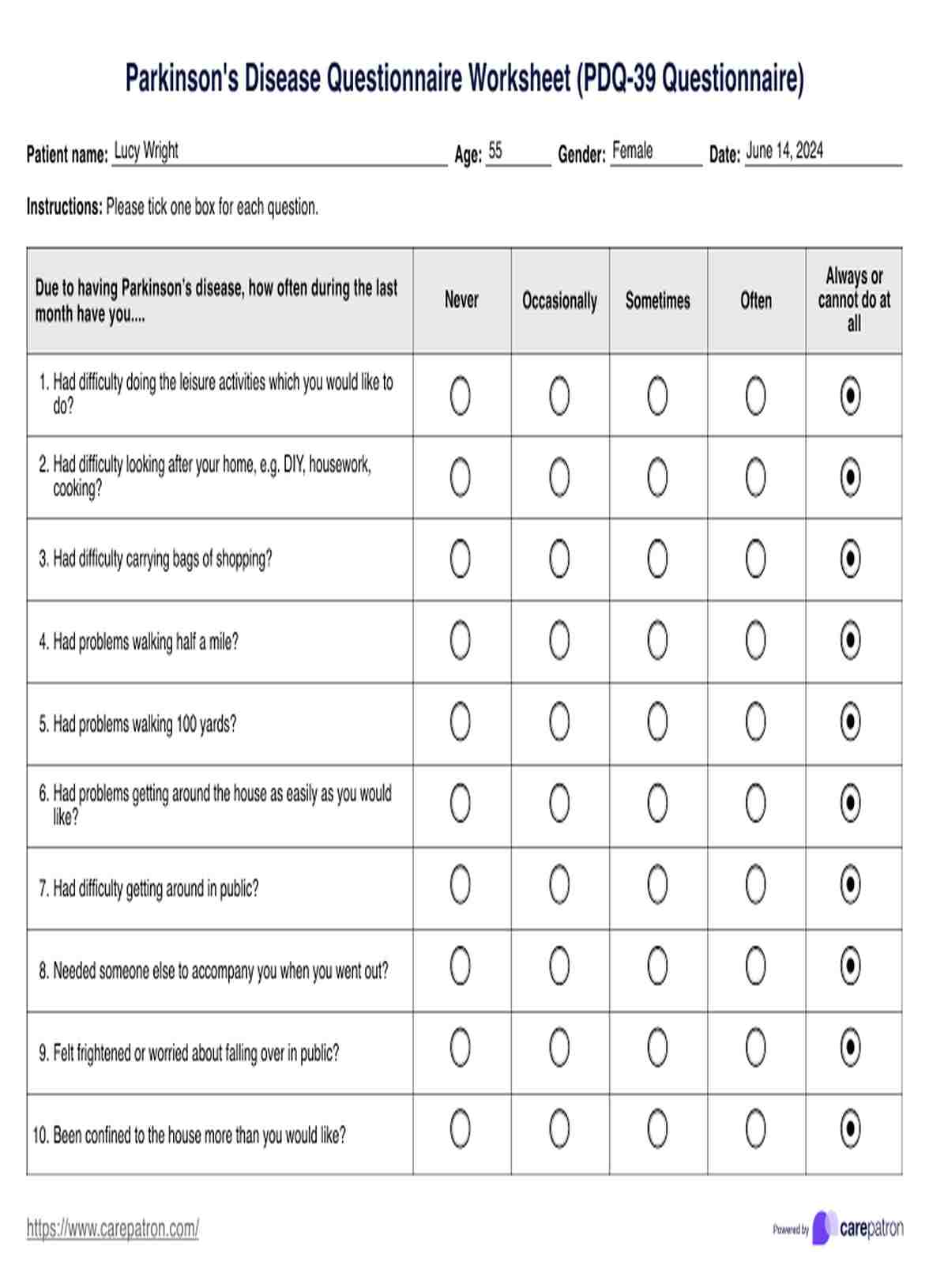
Parkinson's Disease Questionnaire Worksheet
Download a free Parkinson's Disease questionnaire worksheet and example in PDF format to help assess symptoms and track progress. Perfect for patients and caregivers.
Parkinson's Disease Questionnaire Worksheet Template
Commonly asked questions
The Parkinson's Disease Questionnaire (PDQ-39) is a standardized tool designed to assess the health status and quality of life of individuals with Parkinson's disease. It covers both motor and non-motor symptoms to provide a comprehensive evaluation.
Ask about their current symptoms and how they are affecting daily activities. Inquire about their emotional well-being and support network to understand the broader impact of the disease on their life.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











