Collaborative practice agreements are typically written to outline the roles, responsibilities, and scope of practice for nurse practitioners and collaborating physicians. They should address patient care, practice protocols, communication methods, record-keeping procedures, and dispute-resolution processes.
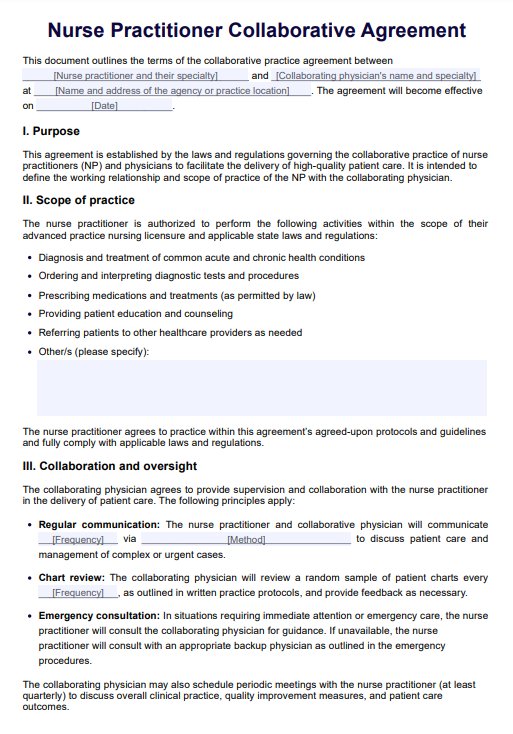
Nurse Practitioner Collaborative Agreement Template
Create a professional Nurse Practitioner Collaborative Agreement Template with our easy-to-use template. Get this for free now to get started!
Nurse Practitioner Collaborative Agreement Template Template
Commonly asked questions
Collaboration between physicians and nurse practitioners involves working together to provide patient care. Physicians offer supervision, diagnosis, consultation, and guidance to nurse practitioners who deliver healthcare services within their scope of practice. The nurse practitioner must practice with the collaborating physician continuously present, especially during the early stages, to provide necessary guidance and support.
A certified registered nurse anesthetist (CRNA) is an advanced practice nurse who administers anesthesia for surgeries and medical procedures.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











