A medical prior authorization is an approval process required by insurance companies before they will cover certain healthcare services or treatments. This helps ensure that the prescribed treatment is necessary and appropriate for the patient's condition.
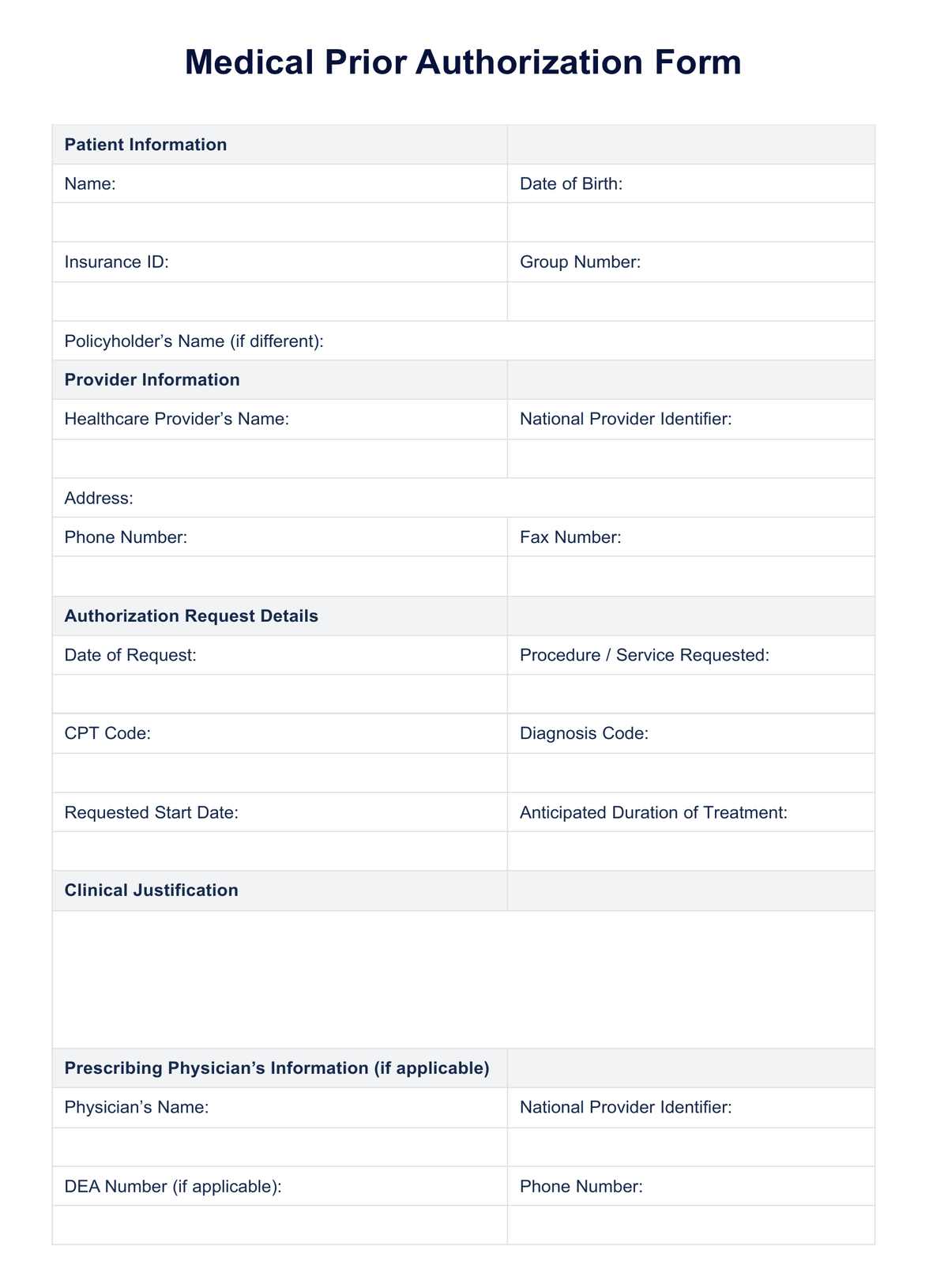
Medical Prior Authorization Form
Learn the importance of prior authorization for your patients. Download a free Medical Prior Authorization Form to simply insurance requests.
Use Template
Medical Prior Authorization Form Template
Commonly asked questions
Insurance companies require prior authorizations to control costs and prevent unnecessary or inappropriate healthcare services from being covered.
Common services that require prior authorization include surgeries, certain medications, diagnostic tests, and medical equipment such as wheelchairs or CPAP machines. Additionally, insurance companies may also require prior authorization for out-of-network providers or specialized treatments.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











