This handout is designed for healthcare professionals like physicians, neurologists, ophthalmologists, and emergency room personnel to aid in recognizing and diagnosing Horner's syndrome.
Horner's Syndrome Diagnosis Guidelines Handout
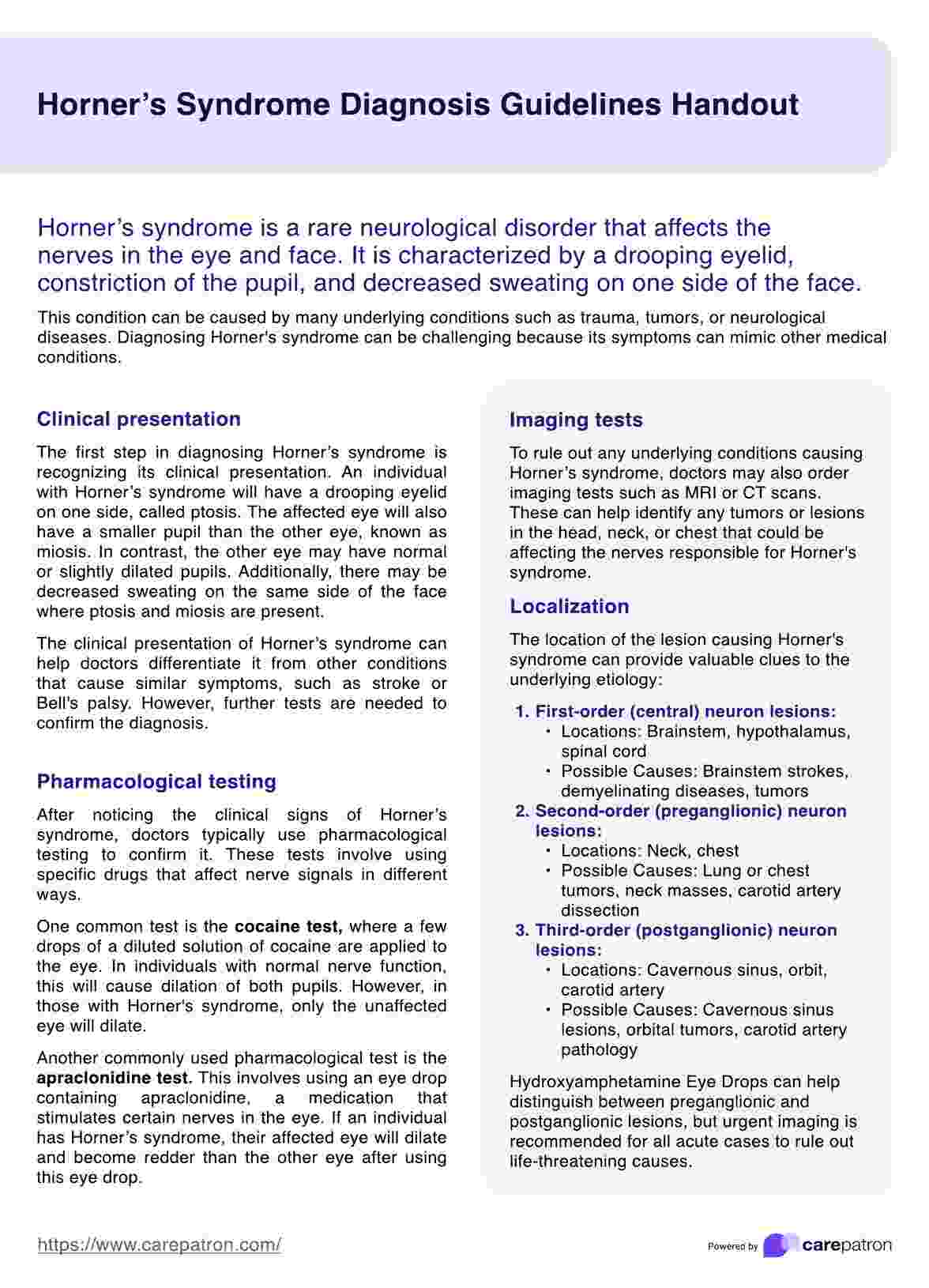
Download our free Horner's Syndrome Diagnosis Guidelines Handout to provide clients with a handy tool for understanding Horner's Syndrome.
Horner's Syndrome Diagnosis Guidelines Handout Template
Commonly asked questions
The handout provides a structured approach to identifying key symptoms, gathering relevant medical history, documenting physical examination findings, and guiding pharmacological testing. It facilitates diagnosis and outlines the next steps for a streamlined approach.
The handout's clear structure ensures that crucial information is efficiently gathered for an accurate diagnosis, saving valuable time and promoting a standardized approach for each patient.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











