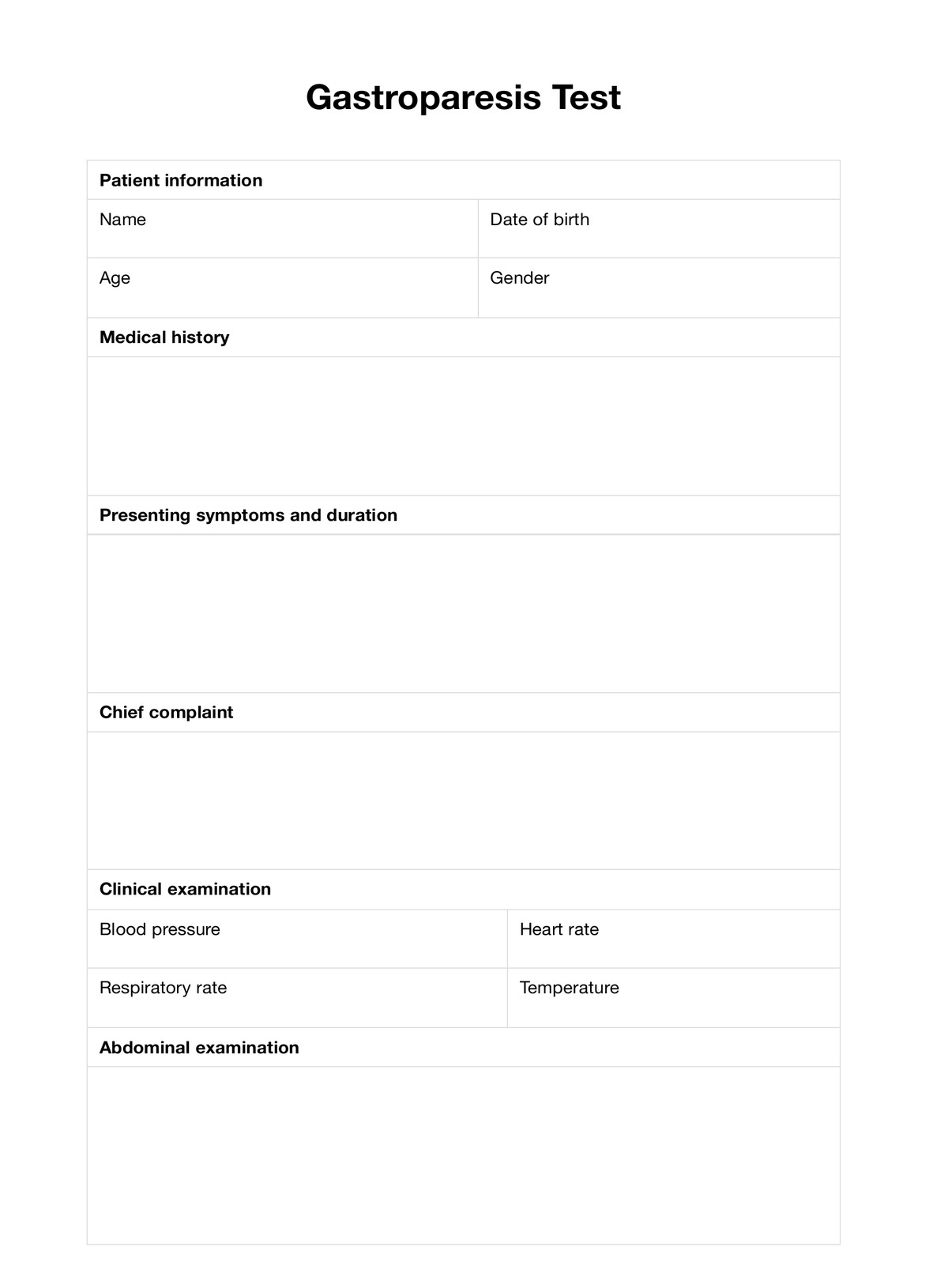
Delayed gastric emptying, commonly known as gastroparesis, is when the stomach takes longer than usual to empty its contents. It often disrupts the upper digestive system's function, leading to symptoms like nausea, vomiting, and fullness after eating small amounts.