A comatose-like state is a deep state of unconsciousness where a person cannot be awakened, fails to respond typically to painful stimuli, light, or sound, lacks a normal wake-sleep cycle, and does not initiate voluntary actions.
Coma Recovery Scale
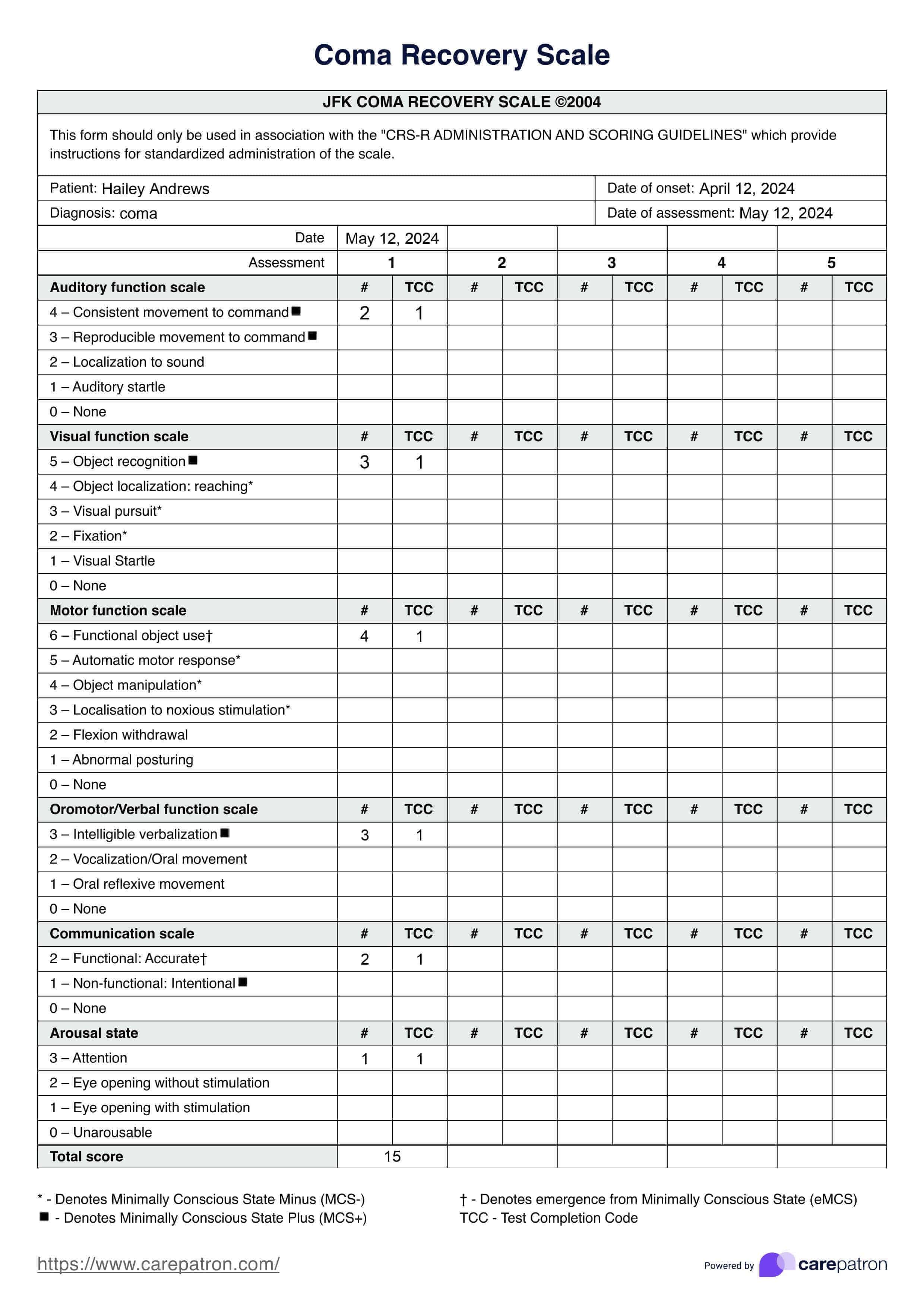
Assess the patient's coma recovery with the Coma Recovery Scale, a standardized tool for evaluating consciousness and predicting outcomes.
Coma Recovery Scale Template
Commonly asked questions
The comatose stage is a clinical condition of deep unconsciousness from which a person cannot be aroused or awakened, resulting from illness, brain injury, or other medical issues. A lack of awareness and response to external stimuli characterizes it.
Comatose levels can vary from light (where some reflex actions may be present and eye-opening can occur spontaneously) to deep (no reflex responses to pain, no spontaneous movements, and no eye-opening).
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











