Normal findings in an upper extremities assessment typically include a muscle strength rating of 5/5, indicating full muscle strength with the ability to resist strong opposition. This demonstrates the individual’s capacity to perform a full range of motion against gravity and resistance without difficulty.
Upper Extremity Strength Assessment
Effectively assess upper extremity strength to gauge physical abilities and use Carepatron's free Upper Extremity Strength Assessment template.
Upper Extremity Strength Assessment Template
Commonly asked questions
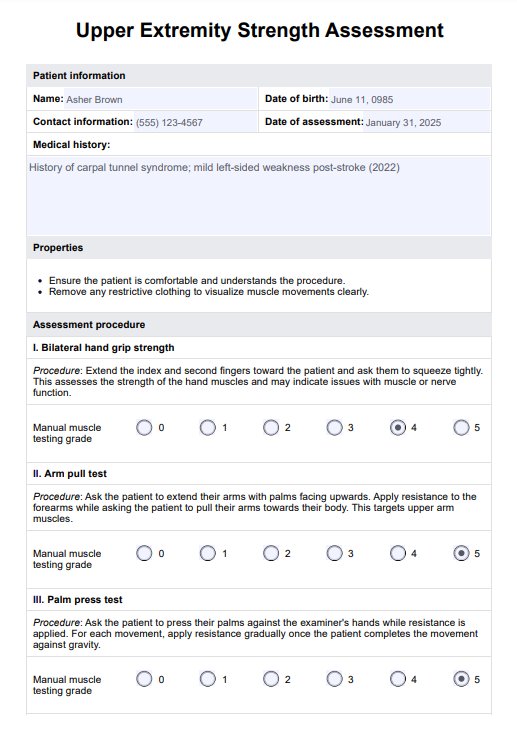
The assessment of upper extremity function evaluates the ability of the shoulders, arms, wrists, and hands to perform tasks that require varying degrees of strength, flexibility, and coordination. It is crucial to determine how musculoskeletal and neurological conditions affect daily living activities.
A muscle strength score of 4+/5 indicates that the individual can perform movements against resistance but not at full strength, showing slightly less than normal capacity. This score suggests that while the muscle is strong, it cannot withstand maximum resistance.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











