In nursing, pain assessment involves systematically evaluating a patient's pain experience. Healthcare providers employ tools like pain scales, inquire about pain characteristics, and consider non-verbal cues, ensuring a holistic understanding of the patient's pain.
Nursing Pain Assessment Template
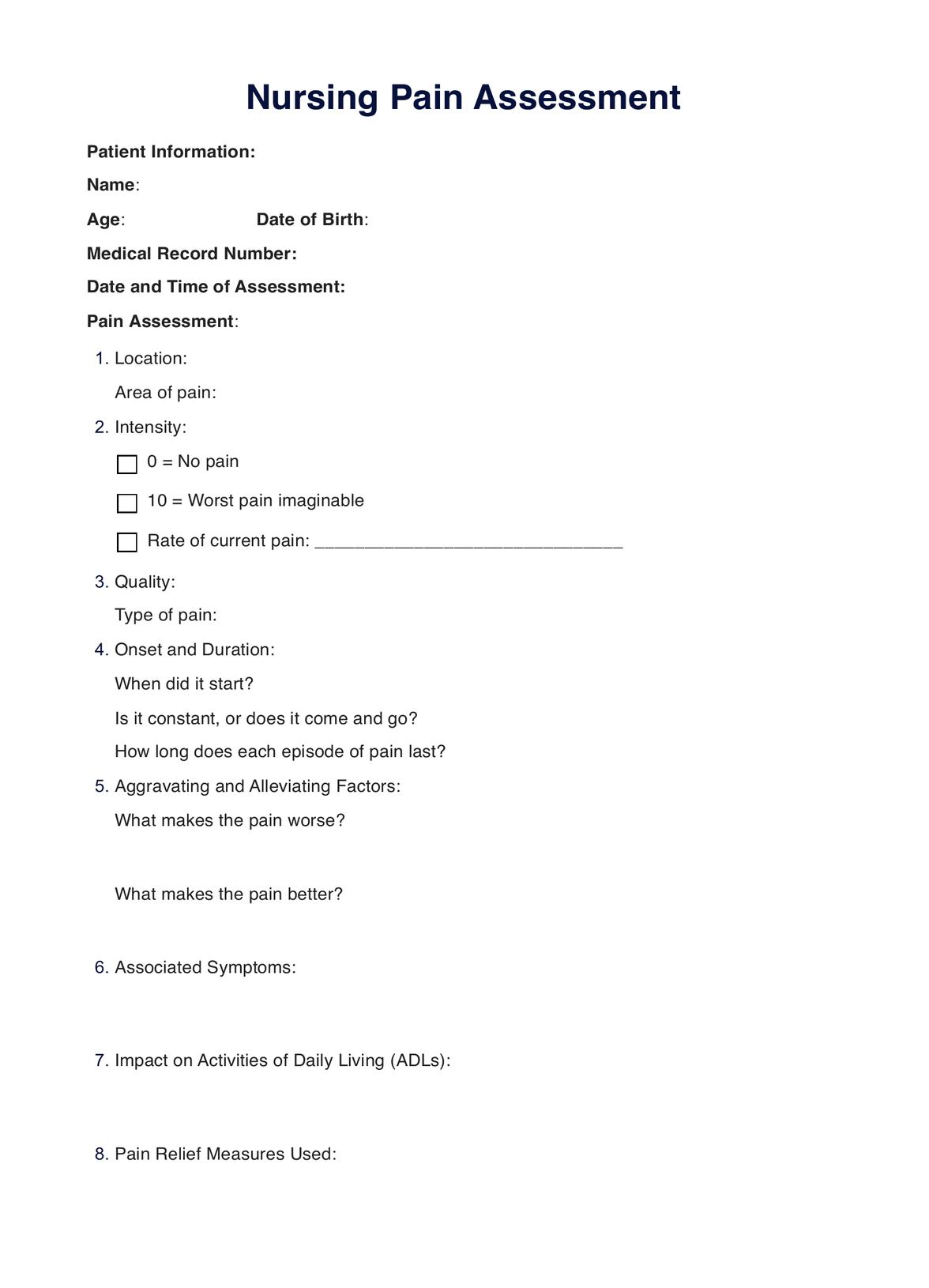
Learn about the importance of nursing pain assessment and how it is carried out in healthcare settings. Download a free PDF example to understand the process better.
Nursing Pain Assessment Template Template
Commonly asked questions
Nursing documentation of pain involves accurately recording details such as pain intensity, location, and factors affecting pain. Carepatron's nursing documentation features provide a seamless platform for healthcare providers to document pain assessments, interventions, and patient responses efficiently.
The five key components of pain assessment include pain intensity, pain quality, pain location, aggravating and alleviating factors, and impact on daily activities.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











