Document clear and symmetrical breath sounds bilaterally, the absence of abnormal breath and any relevant subjective findings.
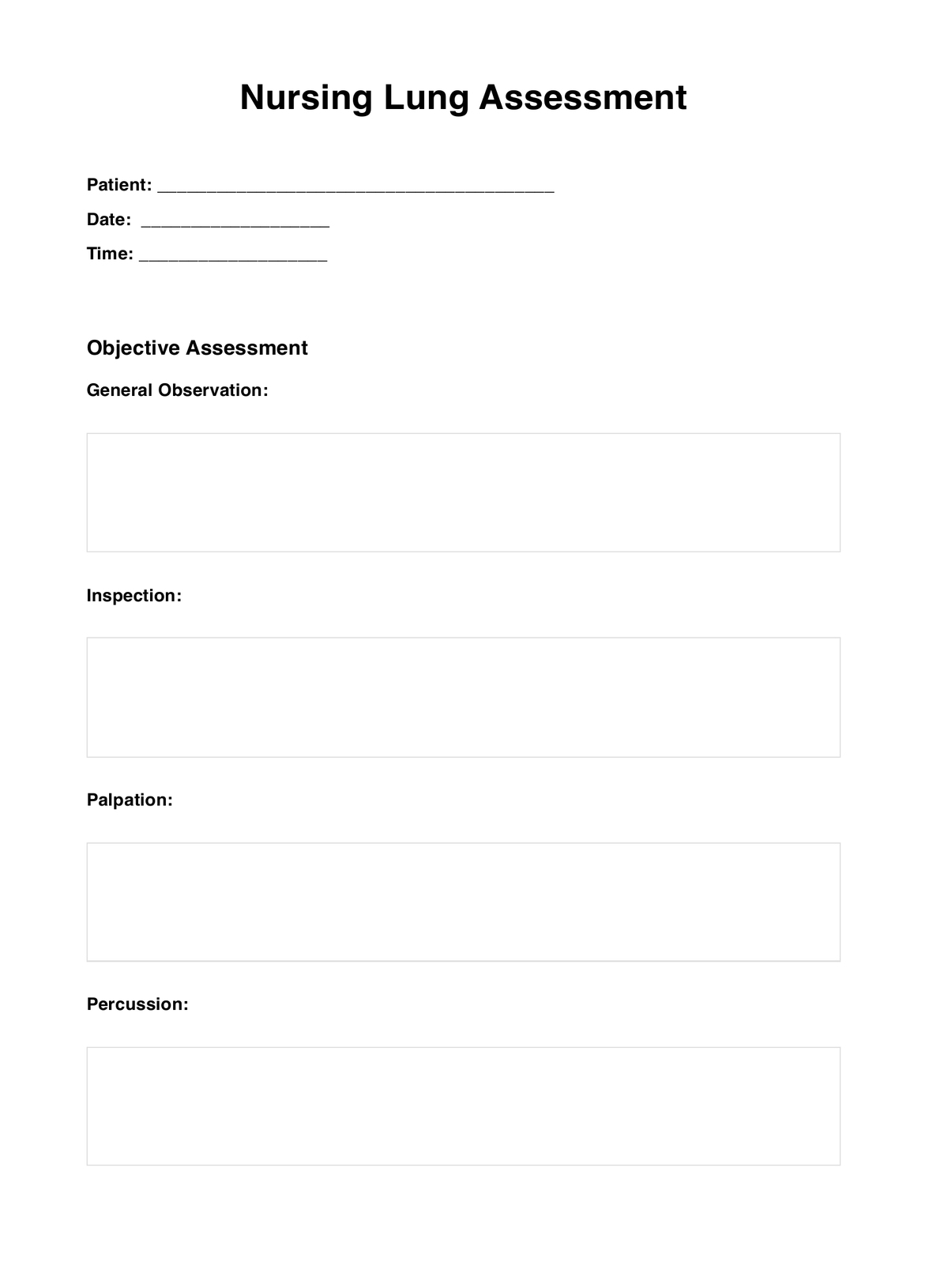
Nursing Lung Assessment
Download this Nursing Lung Assessment to understand the importance of assessing breath sounds, respiratory distress, and signs of respiratory diseases.
Use Template
Nursing Lung Assessment Template
Commonly asked questions
Lung sounds are described based on location, intensity, and quality, using terms such as bronchial, vesicular, wheezes, crackles, and rhonchi.
Components include subjective assessment, inspection, palpation, auscultation, percussion, and voice sound assessment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











