The leading EHR for counselors
Create more space for care. Carepatron’s counseling software combines organization and security, allowing you to focus on creating lasting connections with your clients.

Carepatron’s software for counselors
Carepatron takes the hassle out of managing client sessions. With customizable treatment plans, secure data storage, and integrated communication tools, you'll have everything you need to provide seamless, top-notch care.

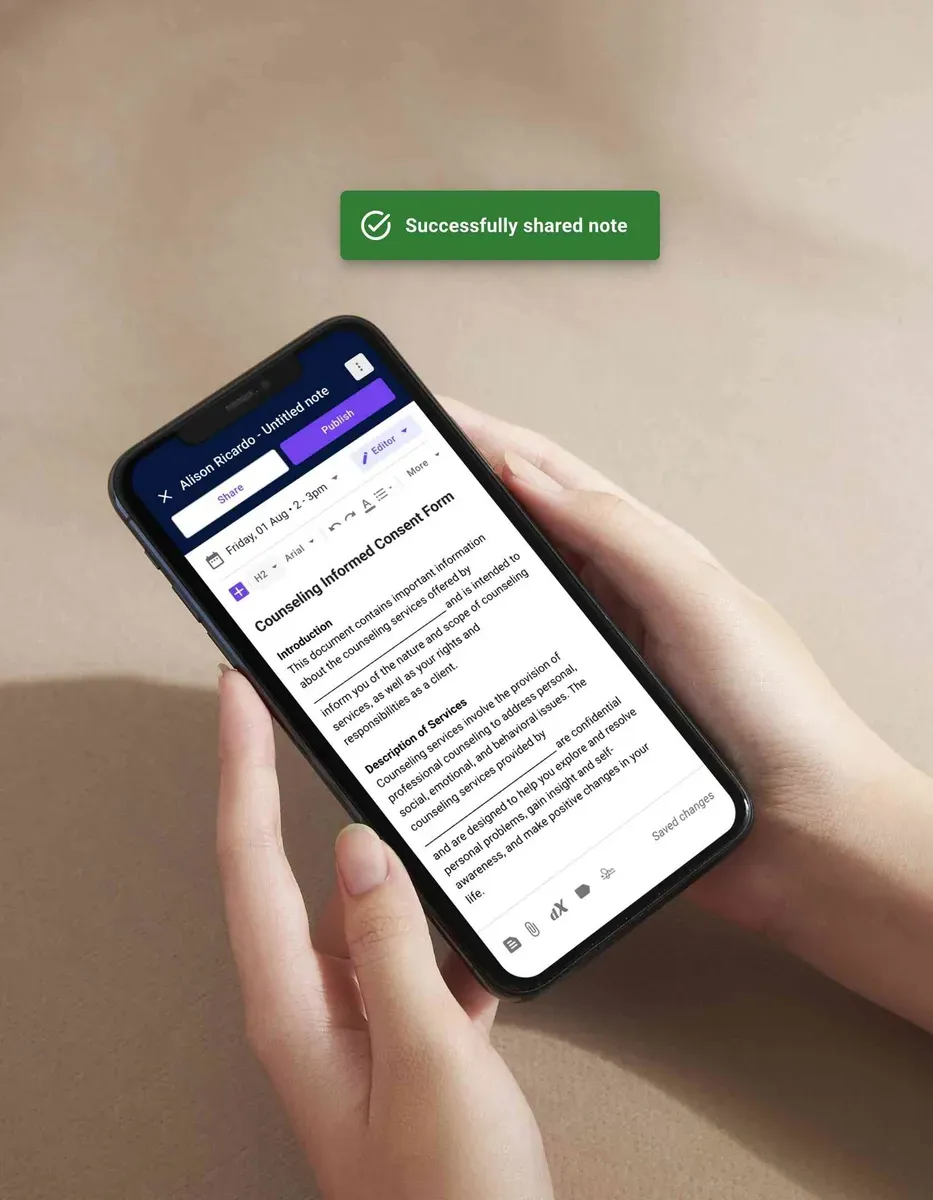
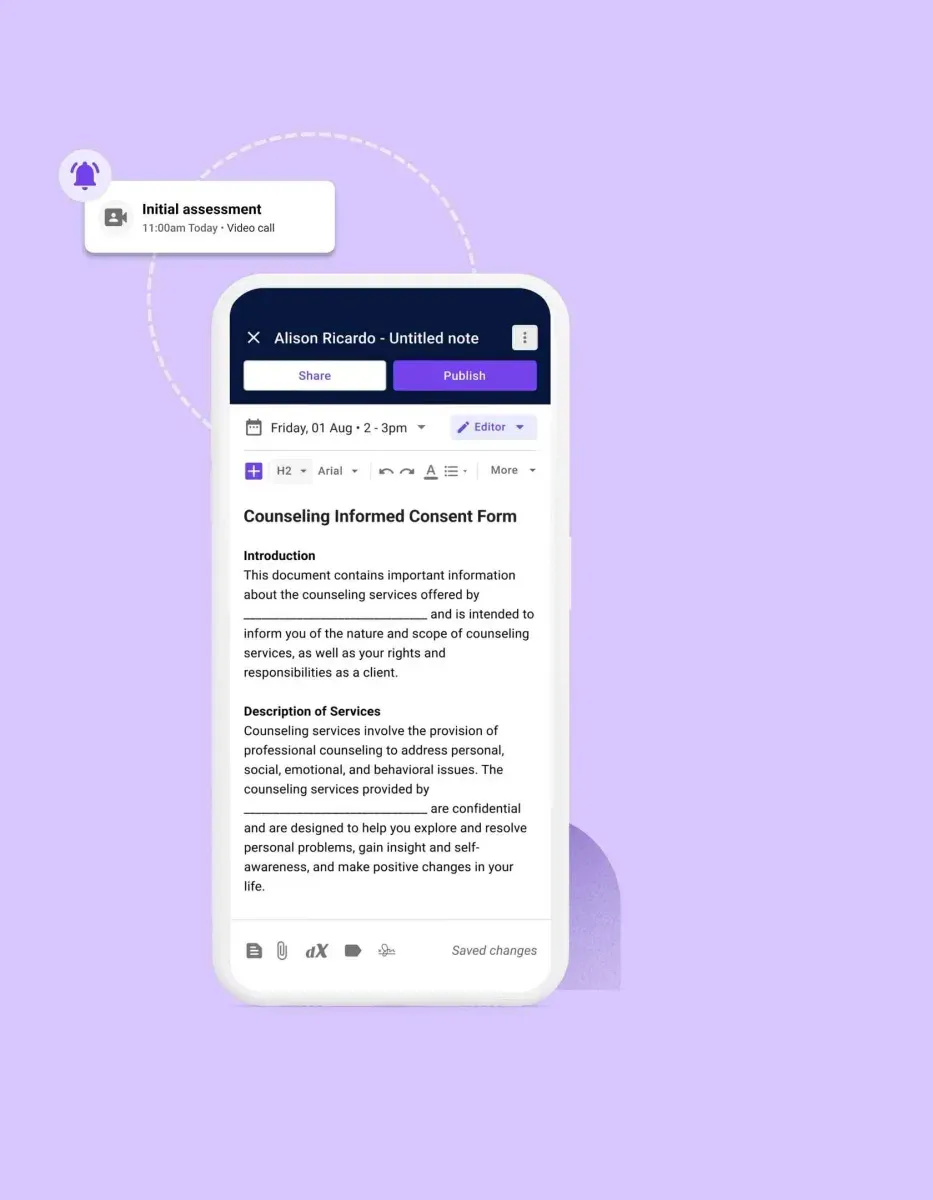
Streamlined note-taking
Effortlessly document client sessions with Carepatron's intuitive note-taking feature. Easily record important details, track progress, and access notes from any device, ensuring seamless continuity of care.

Customizable treatment planning
Tailor treatment plans to each client's unique needs with Carepatron's customizable templates. Guide your practice with structured interventions, goals, and progress tracking, empowering clients to achieve their mental health objectives.

Secure data storage
Rest easy knowing that client data is securely stored with Carepatron's robust encryption measures. Protect sensitive information while maintaining compliance with industry regulations, giving you and your clients peace of mind.

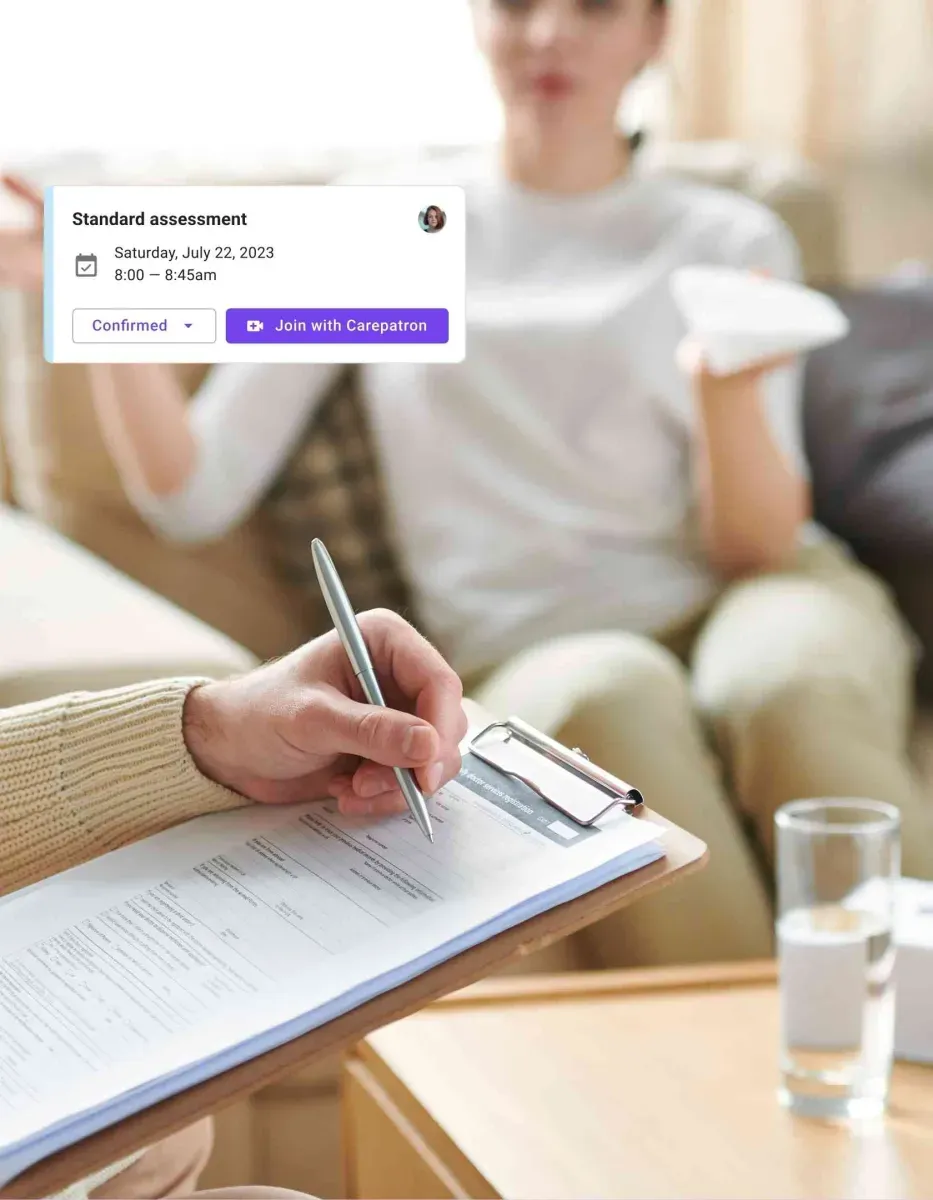
Integrated communication tools
Facilitate seamless client communication through Carepatron's integrated messaging and video conferencing features. Enhance engagement, minimize barriers to care, and foster stronger therapeutic relationships.
Counseling software resources
Access insightful worksheets, expert advice, and industry guidelines. We've curated everything you need to enhance your practice and better serve your clients.
The counseling notes solution for your healthcare team
With Carepatron, your healthcare team can easily manage counseling notes in one place. Advanced features help ensure accuracy and speed, reducing administrative burden and allowing your team to focus on delivering exceptional care.

Enhanced collaboration
Carepatron's counseling notes software facilitates seamless collaboration among healthcare team members. Share notes securely, collaborate on treatment plans, and ensure continuity of care for optimal patient outcomes.

Streamlined documentation
Save time and resources with streamlined documentation processes, ensuring accurate record-keeping and improved workflow efficiency for healthcare providers.

Comprehensive practice management
Carepatron's counseling practice management software streamlines all aspects of your practice, from appointment scheduling to billing. Maximize efficiency, improve workflows, and enhance overall practice performance.

Robust security measures
Rest assured, knowing that sensitive patient information is protected with Carepatron's advanced security measures. Encrypt data, set user permissions, and maintain HIPAA compliance to safeguard patient confidentiality.
Trusted by more than 100,000 practitioners

"It’s so easy to connect with my staff"
CLAIRE, PHYSICAL THERAPIST

"Carepatron saves me 2 hours everyday"
AEGEUS L, HEALTH COACH

"My team loves how simple it is to use"
ANDREA MAGNUS, PRACTICE MANAGER
Carepatron’s counseling software features
Carepatron simplifies your day-to-day by combining scheduling, billing, and client communication in one place. With secure data handling and a platform that adapts to your needs, you can focus on client sessions.

Streamlined operations
Effortlessly manage scheduling, note-taking, and billing all in one place. With Carepatron, you can streamline your administrative tasks, allowing you to focus more on providing quality care to your clients.

Enhanced client communication
Communicate with clients seamlessly through integrated messaging and video conferencing features. Carepatron makes staying connected with your clients accessible, fostering stronger therapeutic relationships and improving engagement.

Secure data management
Safeguard patient information with robust encryption, ensuring compliance with the highest data protection standards. Our secure data management meets and exceeds industry benchmarks, providing a foundation of trust and confidence.

Customizable features
Healthcare teams can change the platform to fit their needs. Personalization and easy adaptation can be integrated into different workflows.
The benefits of Carepatron’s counseling practice management software
Take advantage of Carepatron's counseling practice management software for your practice. Carepatron delivers what you need to succeed, from improved efficiency to enhanced client satisfaction.

Enhanced efficiency
Carepatron's software allows healthcare teams to process payments seamlessly, reducing administrative burden and ensuring timely reimbursements. With automated features like payment reminders, teams can focus more on patient care.

Improved client satisfaction
Deliver a seamless experience for your clients with Carepatron's user-friendly features. From easy appointment scheduling to secure communication channels, Carepatron helps you exceed client expectations and enhance overall satisfaction.

Comprehensive data management
Centralize all your counseling notes and client information in one secure location with Carepatron. Our software ensures easy access to records, facilitates collaboration among team members, and maintains compliance with industry regulations.

Customizable solutions
Tailor Carepatron's features to suit the unique needs of your counseling practice. Whether you need customizable templates for treatment plans or flexible billing options, Carepatron provides the tools to optimize your practice.
Using the counseling software as a mental health practitioner
See how Carepatron’s counseling software can change the way you run your practice. Built with mental health professionals like you in mind, it has all the tools to make your work easier.

Efficient note-taking
Quickly record session notes, assessments, and treatment plans with Carepatron's counseling notes software. Streamline documentation processes to focus more on providing quality care to your clients.

Personalized treatment planning
Tailor treatment plans to each client's unique needs using customizable templates and interventions. With Carepatron's counseling practice management software, you can effectively create personalized strategies to support your clients' mental health journey.

Seamless collaboration
Foster communication and collaboration across your team, breaking down barriers and enhancing efficiency. Our platform enables real-time updates and shared documents, facilitating a smooth flow of information and ideas among team members.

Seamless communication
Facilitate communication with clients through integrated messaging and video conferencing features. With Carepatron, you can easily connect with your clients, fostering stronger therapeutic relationships and improving engagement.

Brief breakdown: How to use our free counseling software
Get started with our free counseling software in just a few easy steps. Learn how simple it is to experience its full potential:

Sign up for an account
Create your free account on our platform by providing basic information. Gain instant access to our counseling software and start optimizing your practice today.

Customize your settings
Personalize your software settings to align with your counseling practice needs. Customize templates, scheduling preferences, and communication channels to enhance efficiency and client satisfaction.

Start documenting sessions
Utilize our counseling notes software to document client sessions seamlessly. Record session notes, assessments, and treatment plans quickly, ensuring comprehensive documentation and continuity of care.

Utilize practice management tools
Take advantage of our counseling practice management software to streamline administrative tasks. Manage appointments, billing, and client communication efficiently, allowing you to focus more on providing quality care.
Frequently Asked Questions
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments