No. It shouldn’t be because you will measure the difference between the navicular bone heights at neutral and while weight is applied to the foot. Though, since conductors usually use a ballpen to mark the navicular tuberosity, patients might feel a mild prickling discomfort. That’s why we recommend using a non-permanent marker instead. With that, they will probably feel tickled instead.
Navicular Drop Test (NDT)
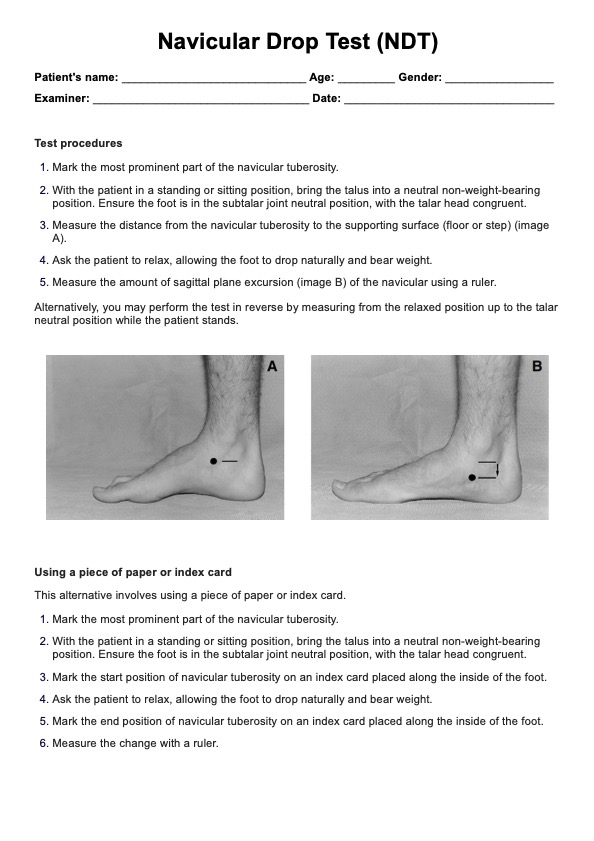
Conduct the Navicular Drop Test (NDT) on your patient’s feet to see if they are overpronated. Overpronation of the foot can lead to problems like Plantar Fasciitis, Achilles Tendonitis, and heel pain! Learn more about this test through this guide.
Navicular Drop Test (NDT) Template
Commonly asked questions
It shouldn’t take more than five minutes, given how simple the instructions are. Though, we do recommend that you be thorough so you can get the best results possible.
Yes. It only gauges foot pronation. It doesn’t pinpoint the exact problem of the foot. Overpronation might be the cause of the problem, but the actual problem can be determined by other physical examination techniques to narrow it down, and imaging tests can be used to confirm it.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











