Spend time with your clients, not your notes
Carepatron's free clinical notes software simplifies documentation, saving you time and enhancing patient care. With access to clinically accurate templates, AI transcriptions, and easy sharing, note-taking has never been easier.

The clinical notes software for your healthcare team
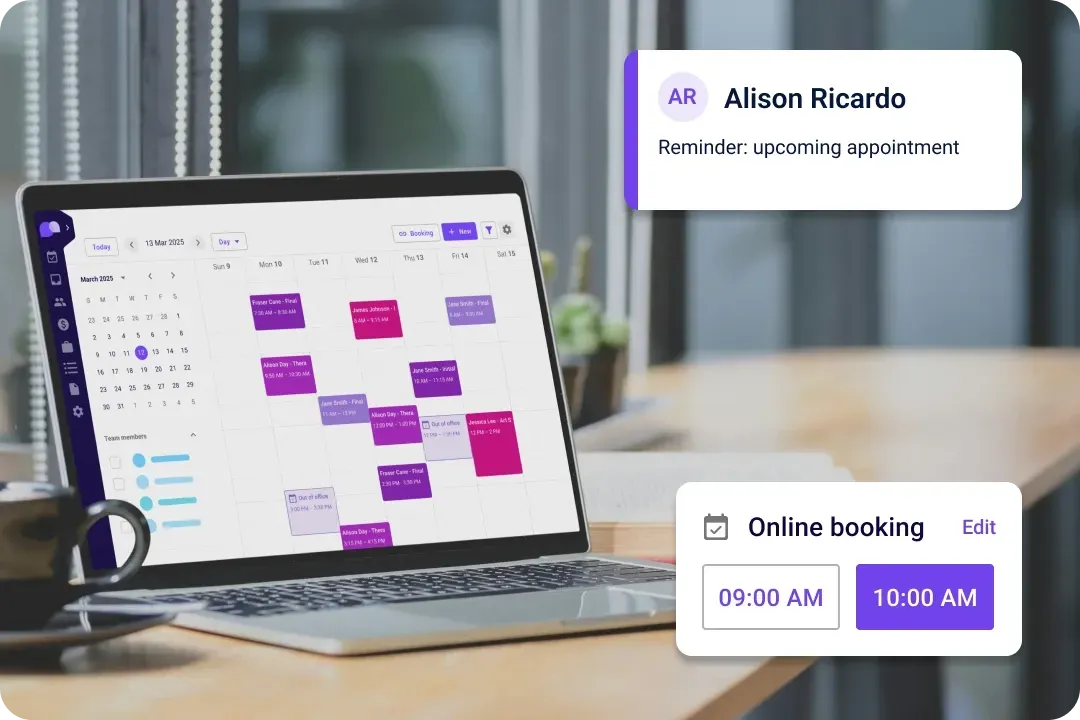
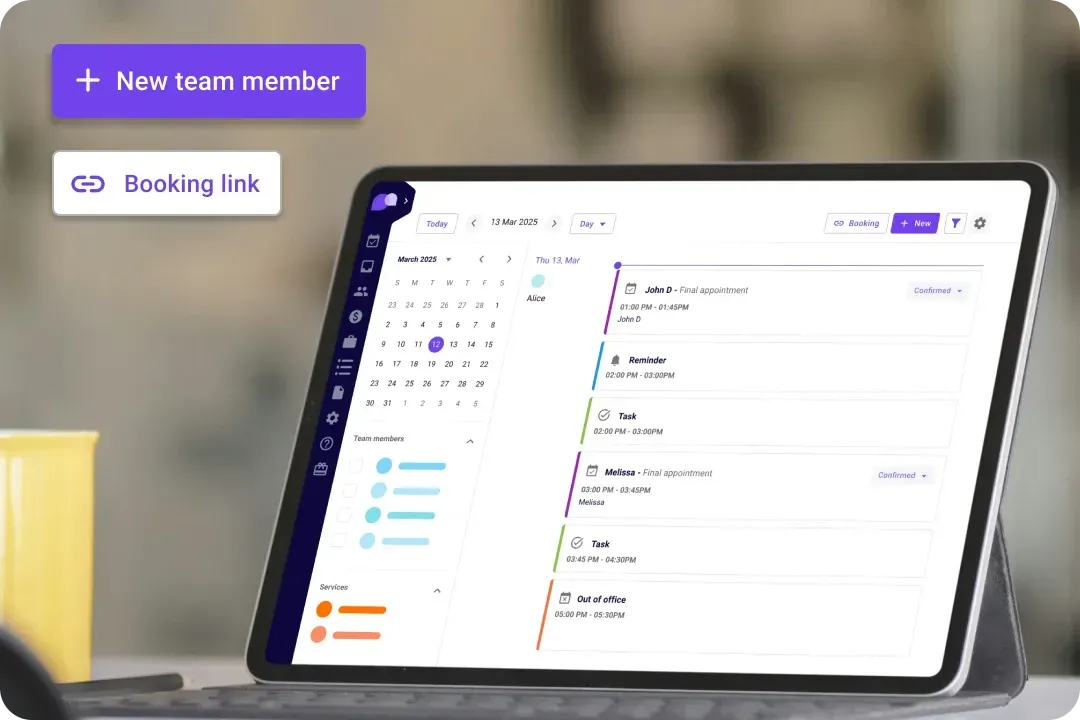
Supercharge your healthcare team with Carepatron's revolutionary clinical notes solution. Designed to boost productivity and streamline your workflow, our user-friendly interface makes creating a clinic note a breeze.

Easy, accurate patient records
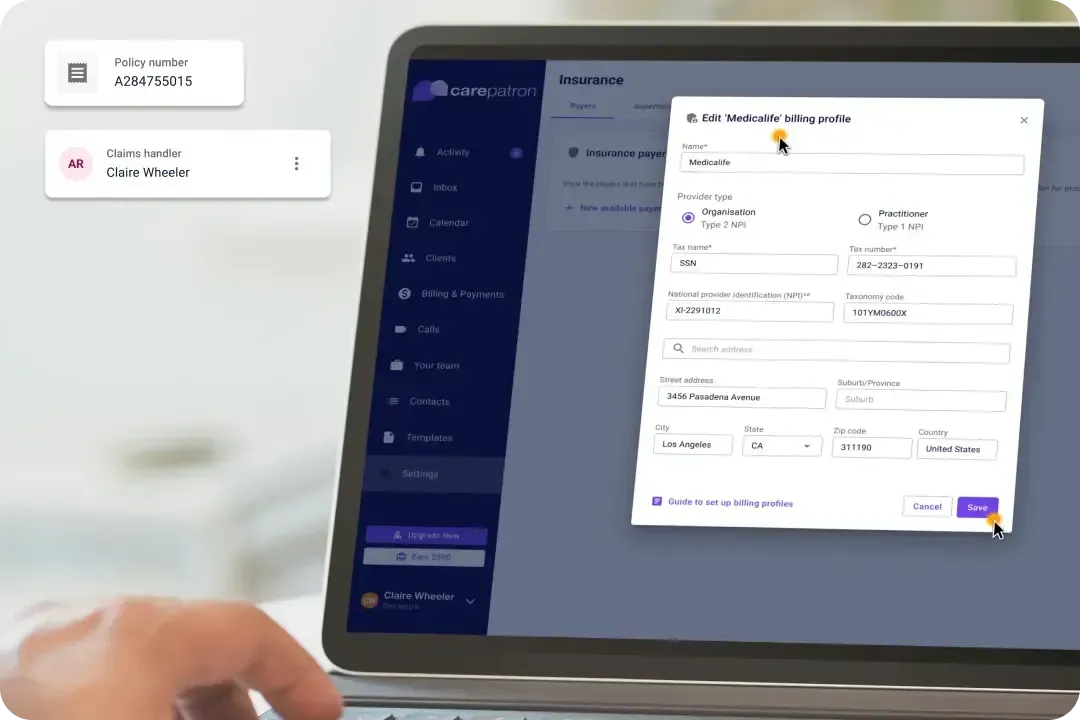
Simplify and streamline patient data management effortlessly with our innovative software platform. Our system integrates electronic health records (EHR) and detailed clinical notes to ensure precise and up-to-date patient history maintenance.

Improved teamwork and efficiency
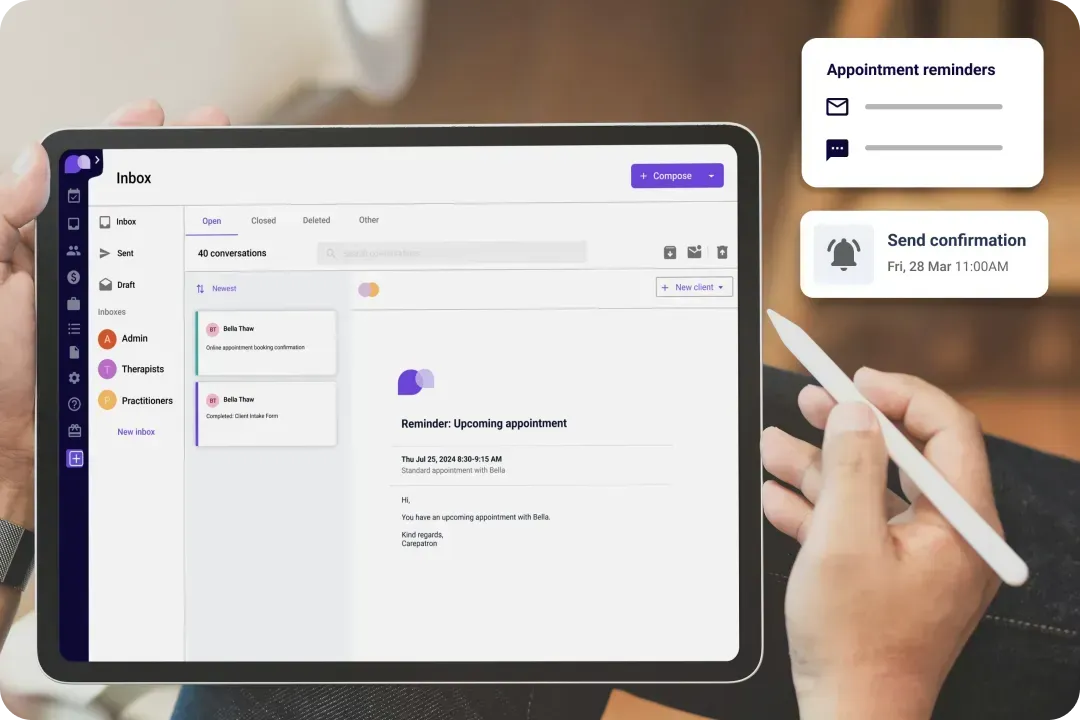
Enhance healthcare teamwork with Carepatron by enabling real-time collaboration on patient files. Healthcare professionals can seamlessly communicate, share insights, and coordinate care plans.

Easy to use–even for non-tech savvy professionals
Carepatron's user-friendly interface ensures quick adoption, even for non-technical users. With clear options, swift navigation, and automated processes, you can seamlessly enhance your practice's efficiency.

Updated security for peace of mind
Fortify data security and compliance with Carepatron's robust measures, keeping patient information safe and secure. Our platform is HIPAA-compliant, ensuring peace of mind for healthcare professionals and patients.
Carepatron’s clinical notes software features
Unleash the power of clinical excellence with Carepatron's user-friendly features that completely transform the way you take clinical notes. Our cutting-edge software seamlessly integrates with your practice management system, ensuring clinic note consistency and eliminating duplication.

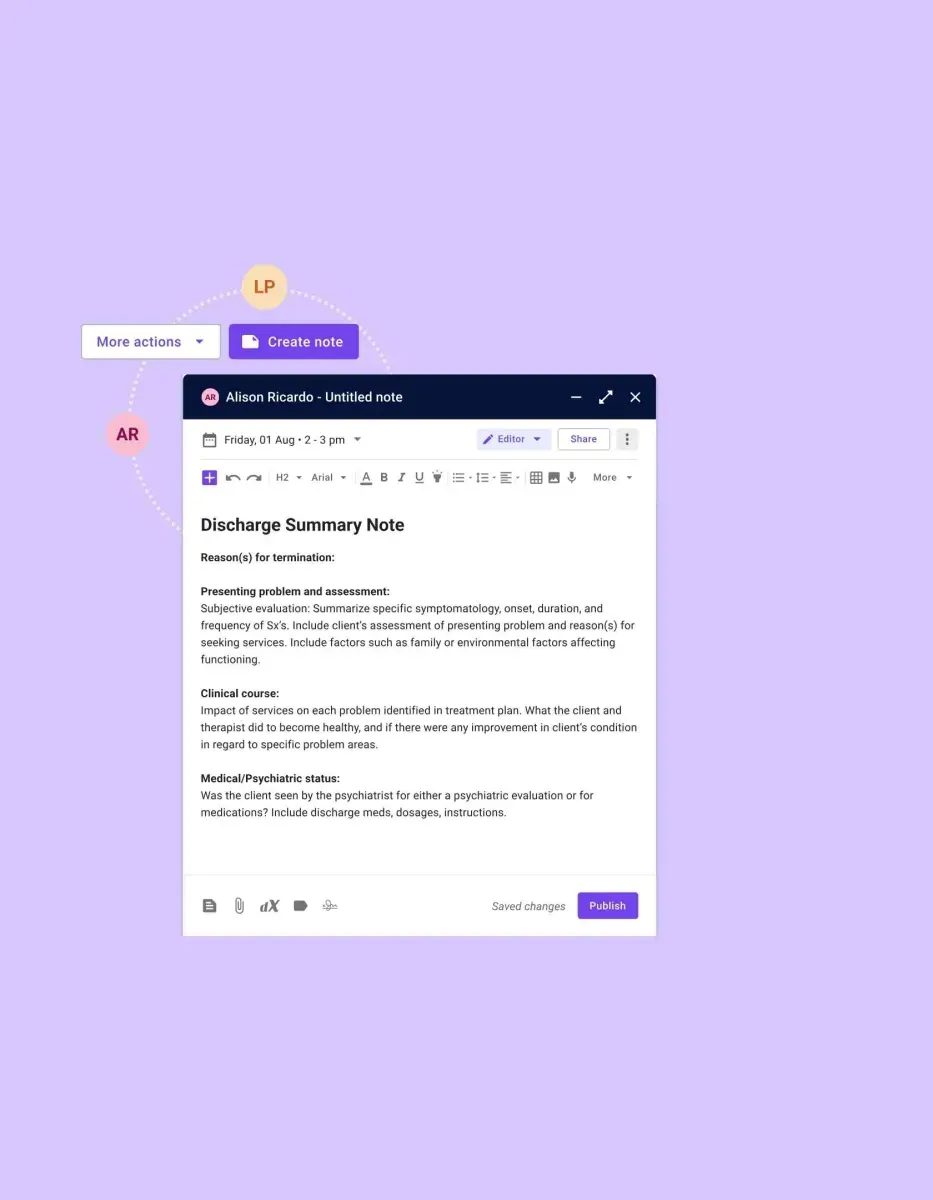
Templates for your unique needs
Elevate your clinic with tailor-made templates to match your needs, streamlining documentation and ensuring patient information capture. Browse our library of templates, from common consultations and examinations to specialized procedures and assessments.

Quick and efficient
Simplify clinical processes with smart search, quickly accessing patient notes and history for all your information needs. Boost productivity and save time with instant, accurate information at your fingertips.

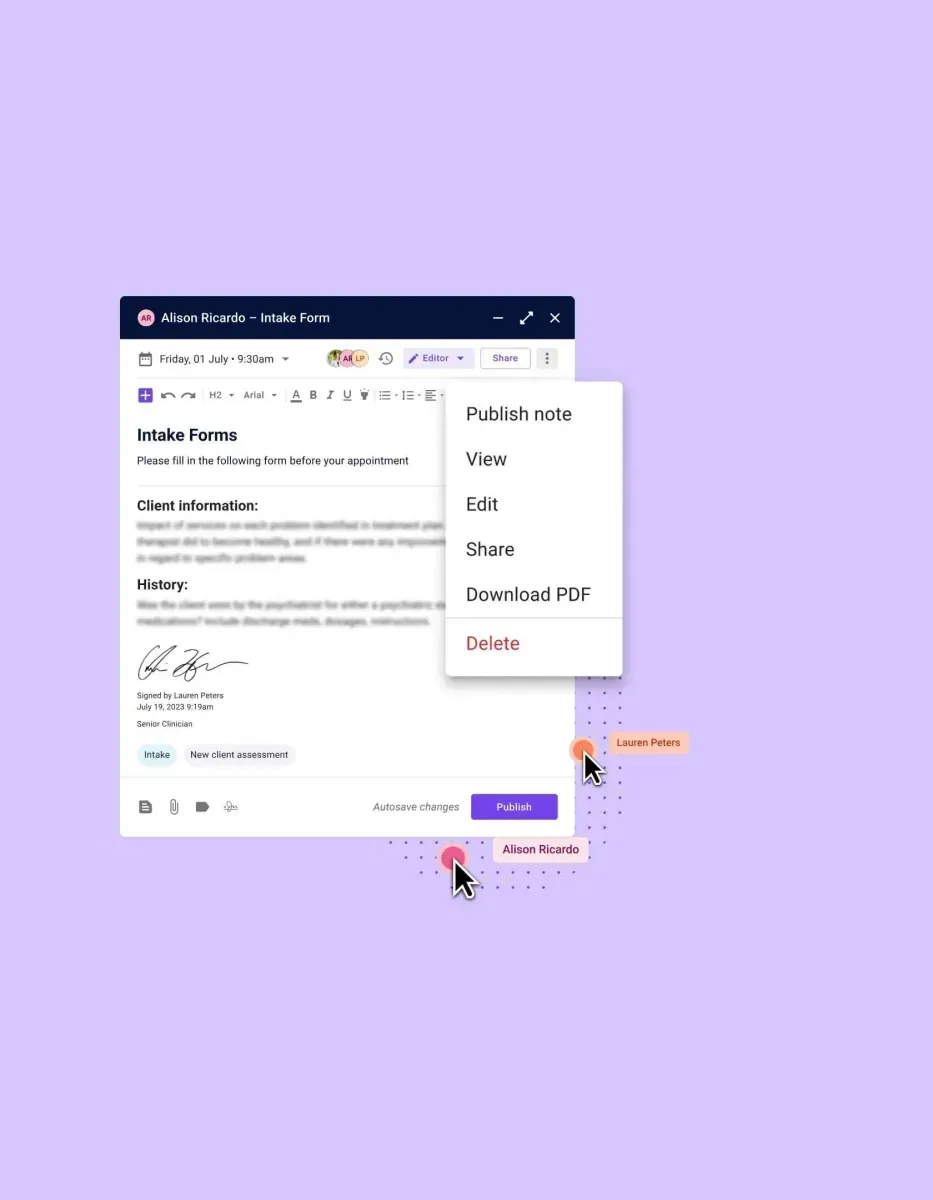
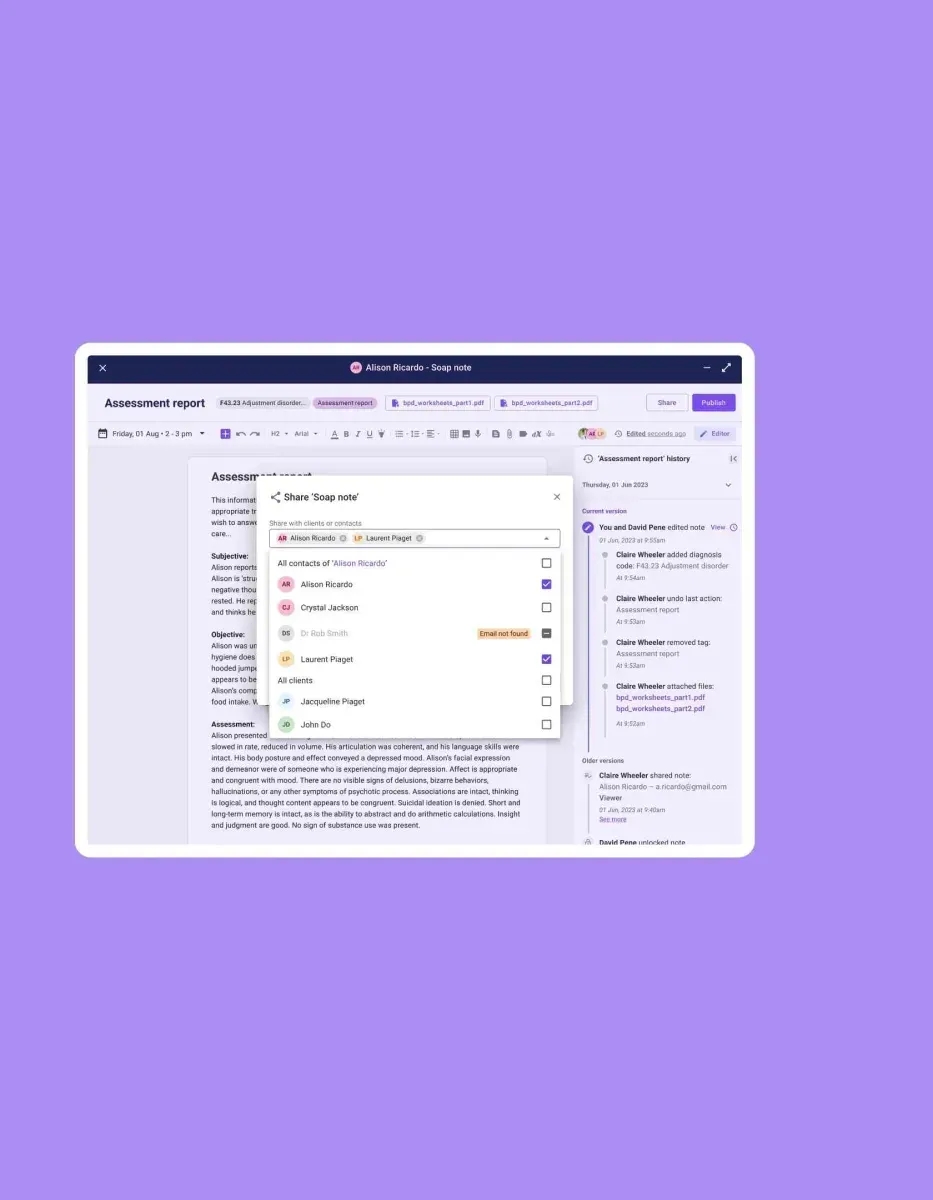
Seamless collaboration with staff
Foster real-time collaboration, enabling multiple providers to collaborate on notes for enhanced teamwork. With Carepatron, you can delegate tasks and share information, ensuring efficient communication.

No manuals required
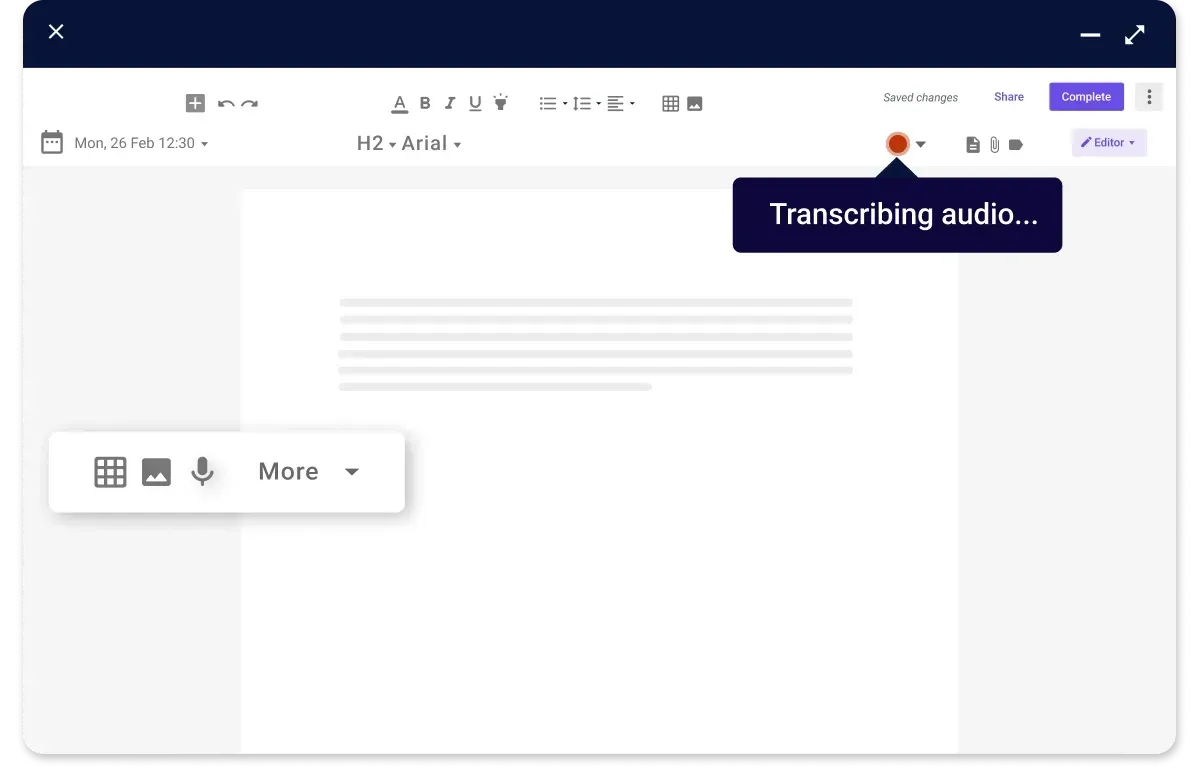
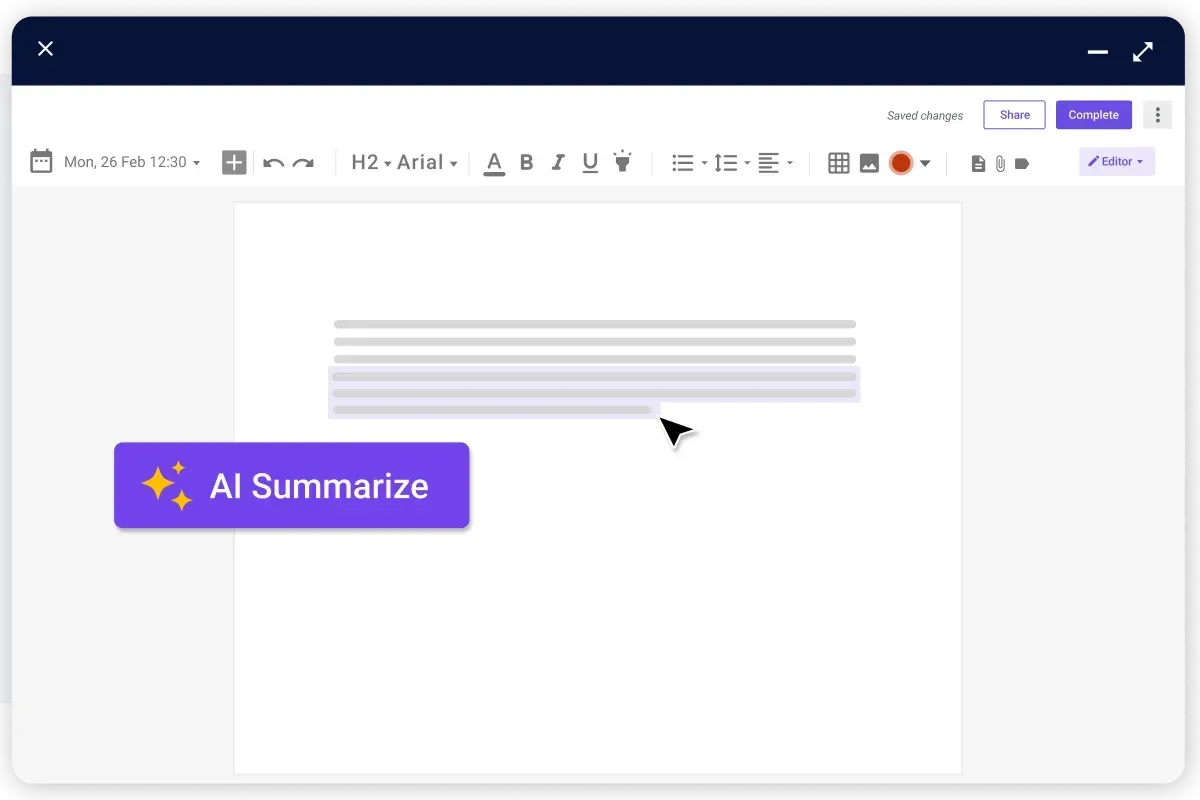
Embrace hands-free note-taking with voice-to-text functionality, optimizing time spent on documentation and maintaining precise records. No need for complicated manual typing or tedious data entry.
Trusted by more than 100,000 practitioners

"It’s so easy to connect with my staff"
CLAIRE, PHYSICAL THERAPIST

"Carepatron saves me 2 hours everyday"
AEGEUS L, HEALTH COACH

"My team loves how simple it is to use"
ANDREA MAGNUS, PRACTICE MANAGER
How does our clinical notes software help you?
With Carepatron's clinical notes software, you can say goodbye to messy and incomplete patient records. Our solution makes errors a thing of the past as you enjoy streamlined, secured, and superior clinic note functionalities.

Reduced errors without sacrificing quality
Fast track clinical record accuracy using predefined templates, minimizing errors and enhancing the quality of patient documentation. Ensure accurate and complete data entry with customizable templates for your needs.

More time for your patients
Cut down on time with voice-to-text for hands-free note-taking, empowering you to prioritize patient care. You can quickly and accurately document patient encounters, freeing up time for meaningful interactions with patients.

Suitable for small or large teams
Foster teamwork in treatment through simultaneous access and updates to clinical notes by multiple team members, ensuring well-coordinated care. Create a seamless workflow and improve efficiency with our flexible and scalable system.

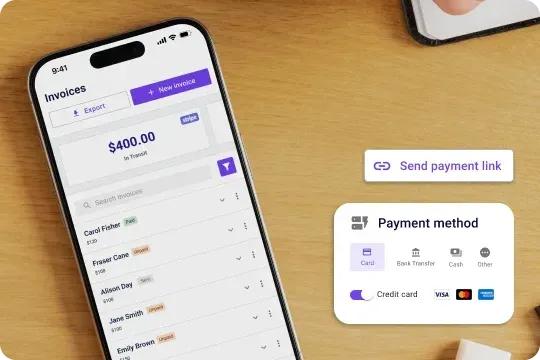
HIPAA-compliant for your safety
Store patient information on our HIPAA-compliant platform for utmost confidentiality and data security. Our system follows strict HIPAA regulations, providing peace of mind for both you and your patients.
The patient notes solution for all healthcare teams
Whether you're a primary care physician, mental health therapist, or specialist surgeon, Carepatron has you covered for every clinic note you have to create. Our clinical notes software adapts to varied healthcare fields with ease.

For all-around comprehensive care
Streamline patient encounters by quickly capturing medical histories, treatment plans, and follow-ups. Elevate the patient experience with access to all of their medical information, including lab results and prescribed medications.

Physical therapy treatments made simple
Document progress notes with ease, track patient rehabilitation, and customize physical therapy plans. Use the latest technologies to help patients achieve their treatment goals and improve their overall health.

Simply note-taking during therapy sessions
Utilize tailored templates that respect the nuances of care, facilitating deeper patient insights and monitoring. With our comprehensive note-taking feature, you can focus on your clients and provide better care.

On-the-go operation notes
Access operative reports and post-surgery notes on-the-go, enabling a focus on precision and patient recovery trajectories. Carepatron's digital platform lets you take notes and review patient progress anytime, anywhere.
Brief breakdown: how to use our clinic notes software
Organizing your clinical notes is as easy as A-B-C with Carepatron:

Choose your note
Create a new note or choose an existing one from your patient's profile. Make sure to enter all the details that you feel are relevant to your patient's care. This will help you keep track of your patient's progress.

Save and store your data
Save and securely store your patient's notes on our encrypted platform, ensuring they are easily accessible anytime and anywhere for future reference.

Find the best template for your needs
Select the appropriate template and customize it to your specific needs. Browse through our selection of templates designed for healthcare professionals.

Take advantage of our tools
Utilize our advanced features, such as voice-to-text or AI medical scribe, and complete your note in record time. These tools help streamline your documentation process and improve accuracy, allowing you to spend more time on patient care.
Frequently asked questions
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments