Smarter billing to save you time
Cut your billing time in half. Carepatron's billing solution turns complicated financials into a few simple clicks. Get paid faster, stress less.

The free medical billing software for your healthcare team
Unlock efficiency and accuracy in financial management with our comprehensive billing solution. Designed to enhance your team's productivity:

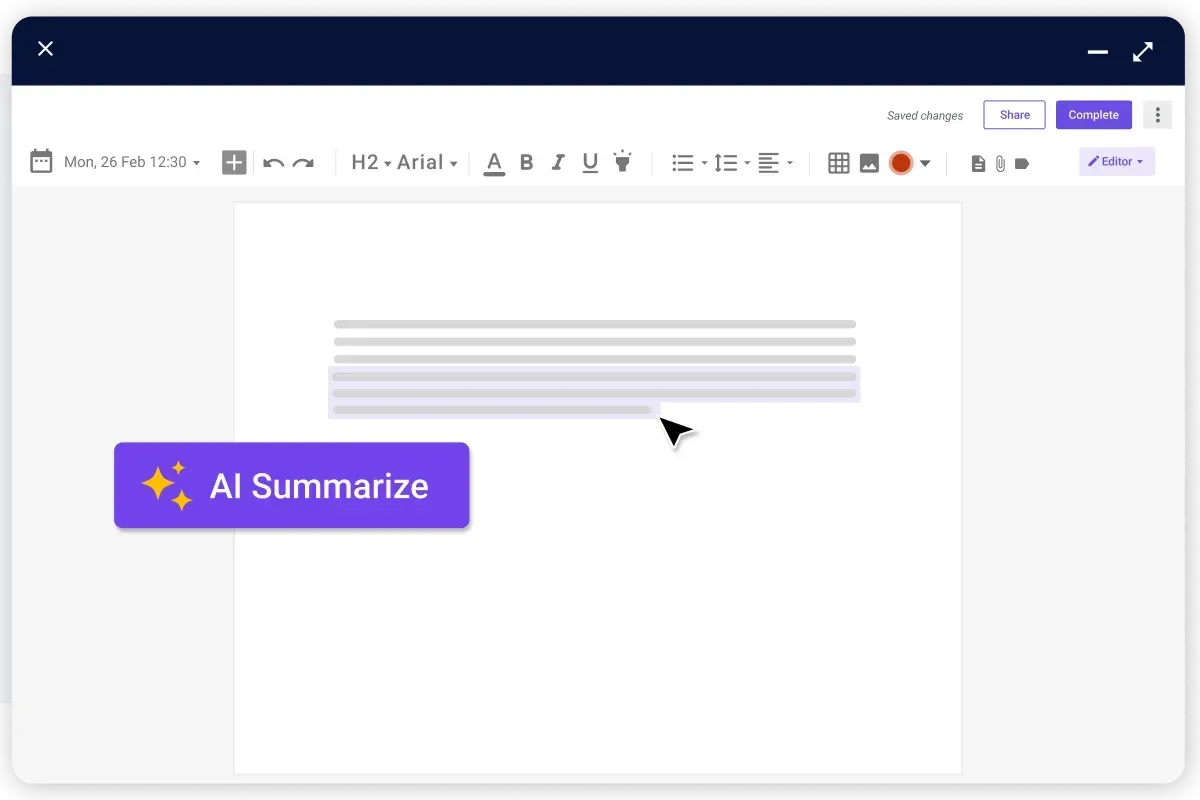
Automates routine tasks
Our comprehensive billing solution significantly reduces manual input by automating routine financial management tasks. This automation boosts your team's productivity, allowing them to focus on what matters most.

Minimizes errors
By ensuring accuracy in billing, our software effectively minimizes errors. This precision safeguards your financial operations against costly mistakes, maintaining the integrity of your billing process.

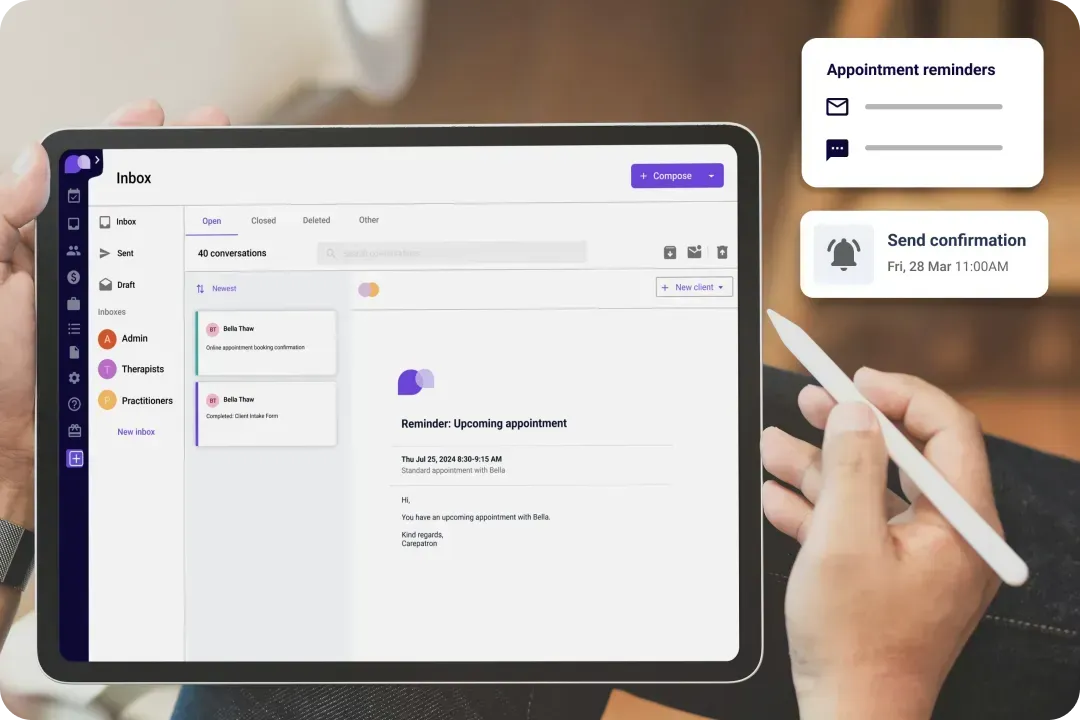
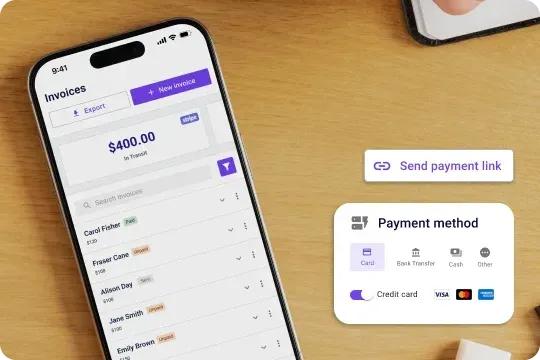
Ensures timely payments
Improving cash flow is crucial for any healthcare practice, and our solution facilitates timely payments. This feature enhances your practice's financial stability by ensuring that revenues are received promptly.

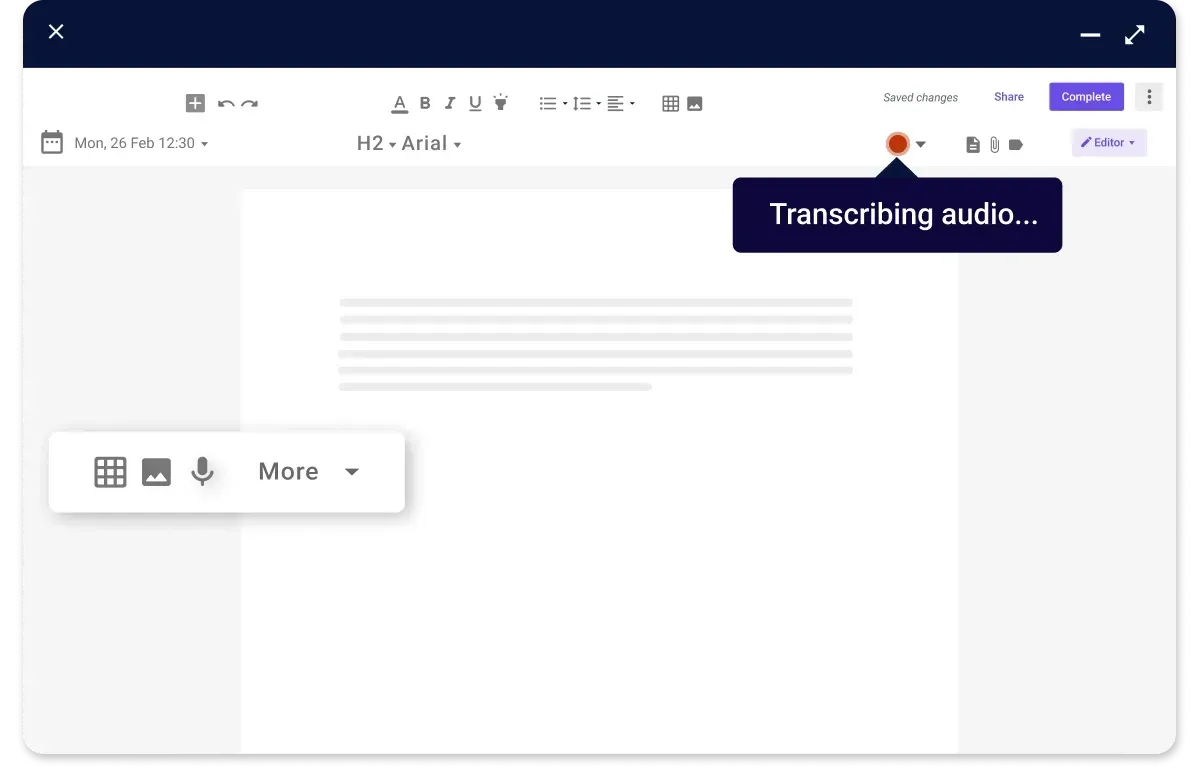
Focuses on patient care
Our billing solution allows your healthcare team to devote more attention to patient care by alleviating financial concerns. This focus ensures that financial management is independent of the quality of patient service.
Carepatron’s online medical billing software features
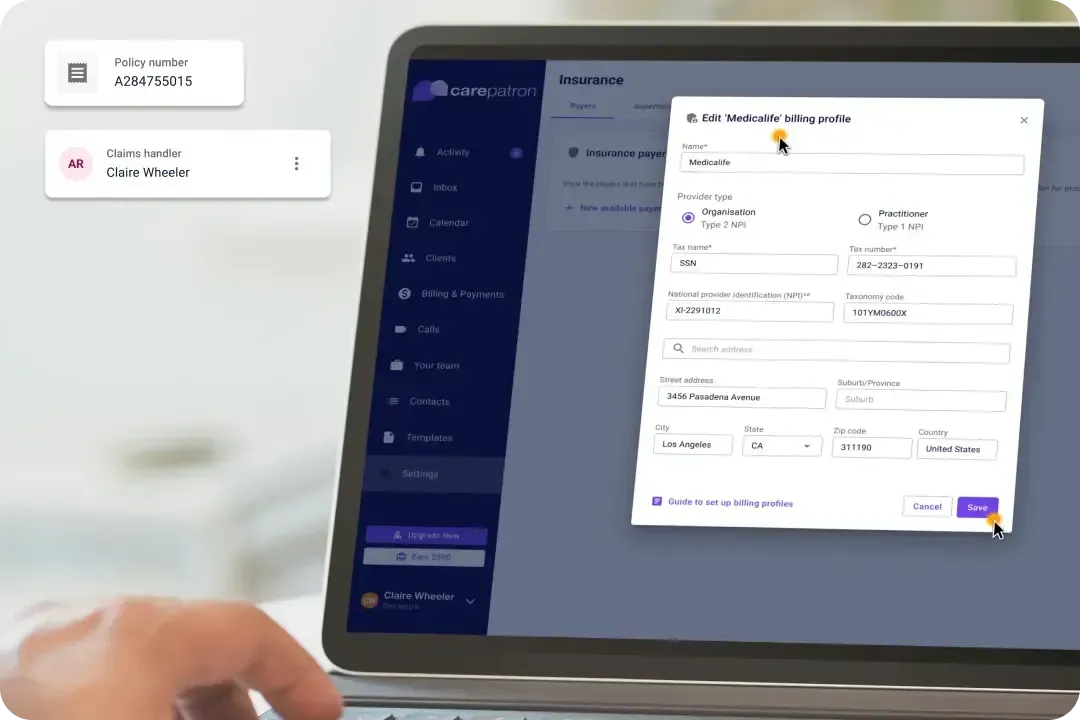
Discover the convenience of advanced billing features with Carepatron. Our medical billing software free plan offers a seamless financial management experience:

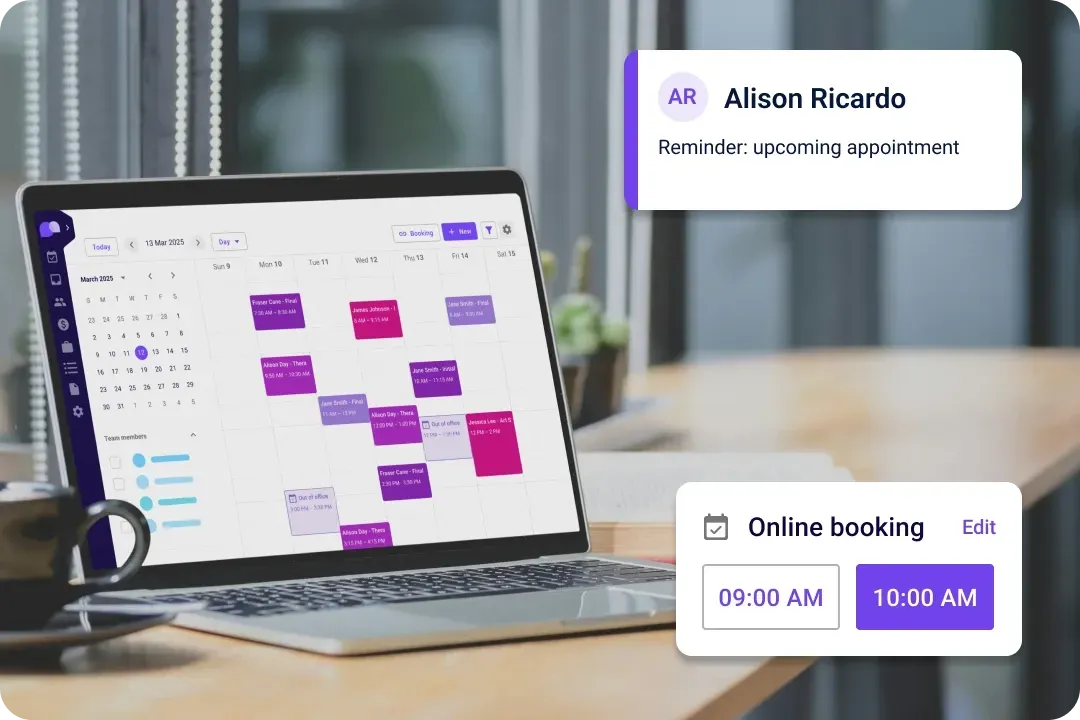
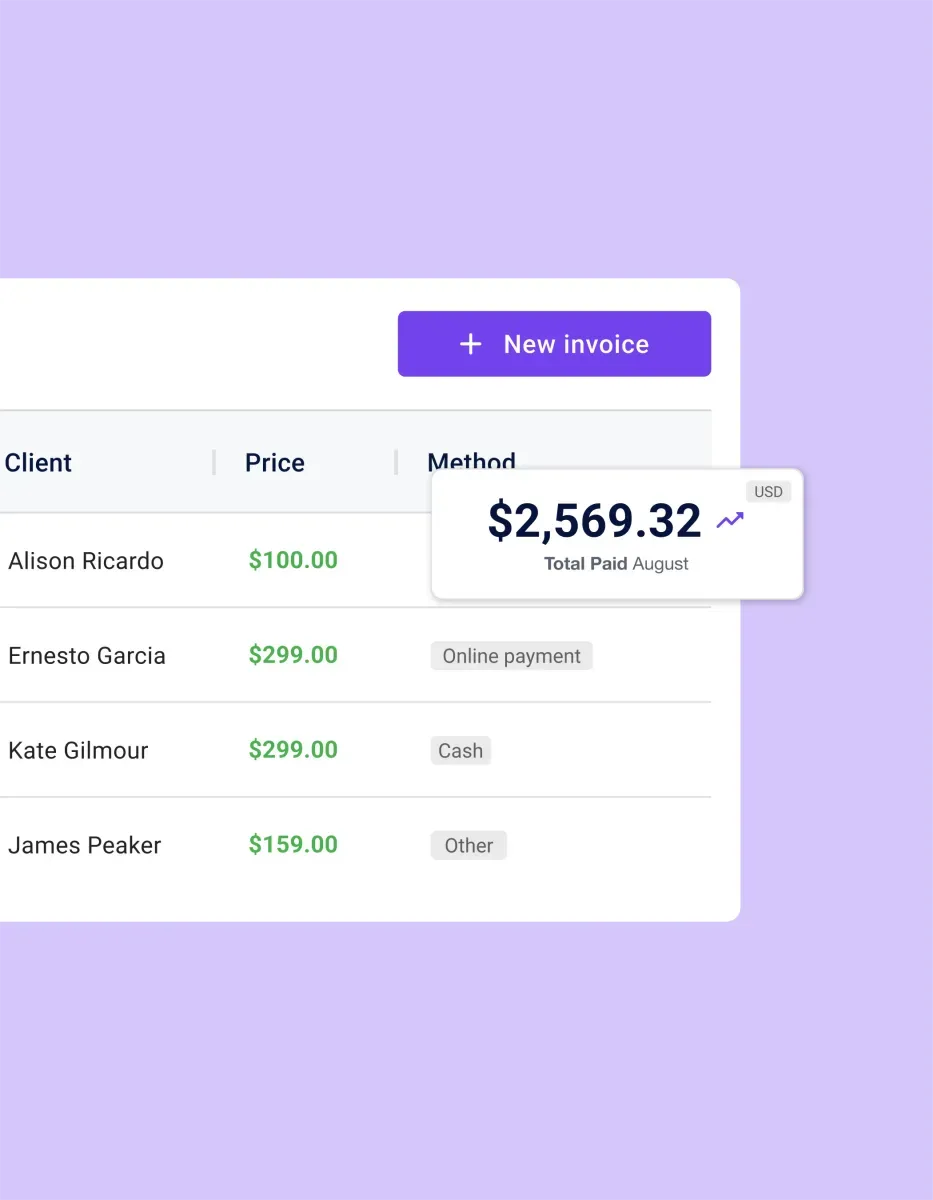
Automatic billing
Experience streamlined processes with automatic billing. This feature simplifies the billing cycle, reducing the time and effort required to manage financial transactions.

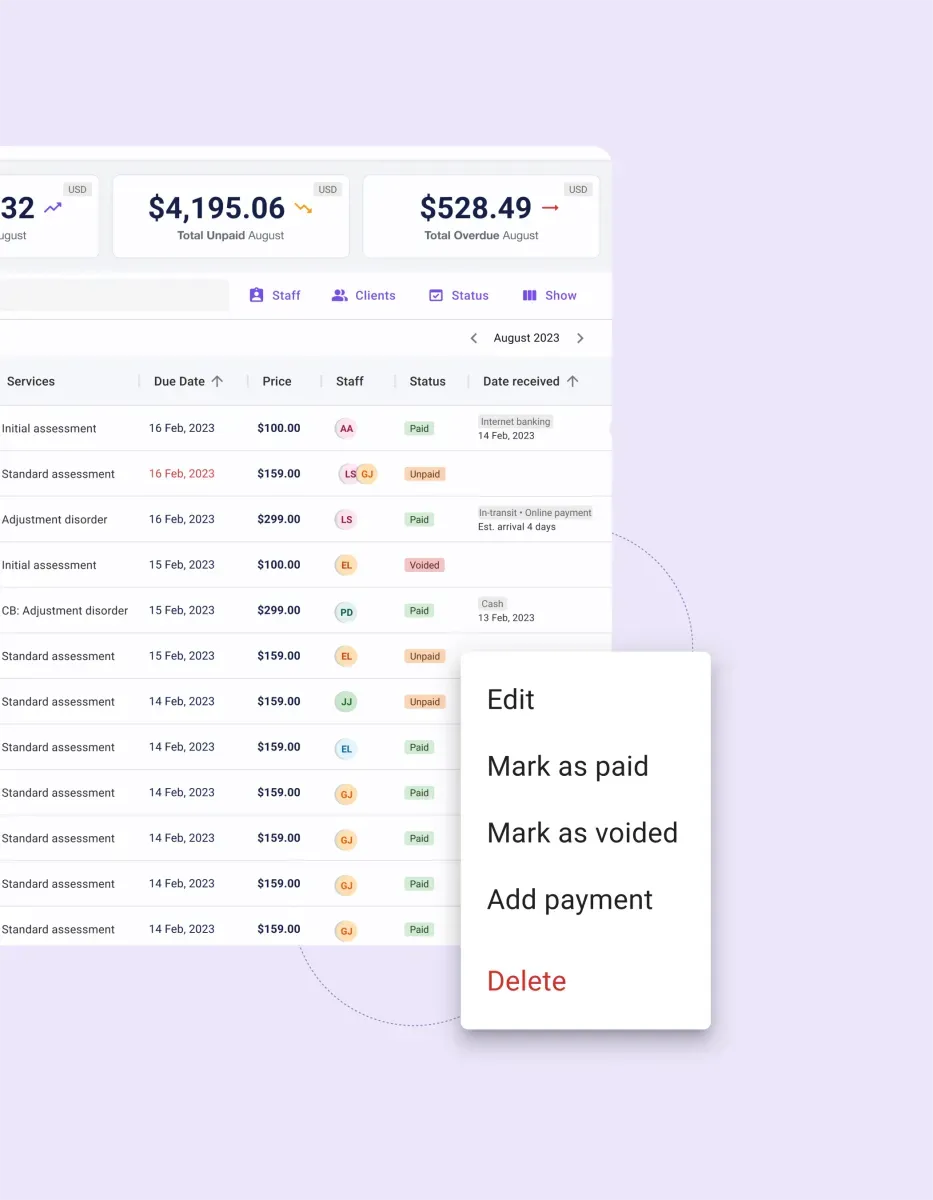
Detailed financial reporting
Gain clear visibility into your practice’s financial health with detailed financial reporting. This transparency allows for better decision-making and financial planning.

Easy claim submission and payment tracking
Our software simplifies claim submission and payment tracking, ensuring that every financial transaction is accounted for accurately and efficiently.

Customizable billing options
Tailor your billing system to fit your practice’s needs perfectly with customizable billing options. This flexibility ensures that our software adapts to your specific financial management requirements.
Trusted by more than 100,000 practitioners

"It’s so easy to connect with my staff"
CLAIRE, PHYSICAL THERAPIST

"Carepatron saves me 2 hours everyday"
AEGEUS L, HEALTH COACH

"My team loves how simple it is to use"
ANDREA MAGNUS, PRACTICE MANAGER

The free medical coding software for every healthcare practitioner
Carepatron’s free medical billing software for small business and practices is engineered for adaptability, supporting a wide range of healthcare services with ease:

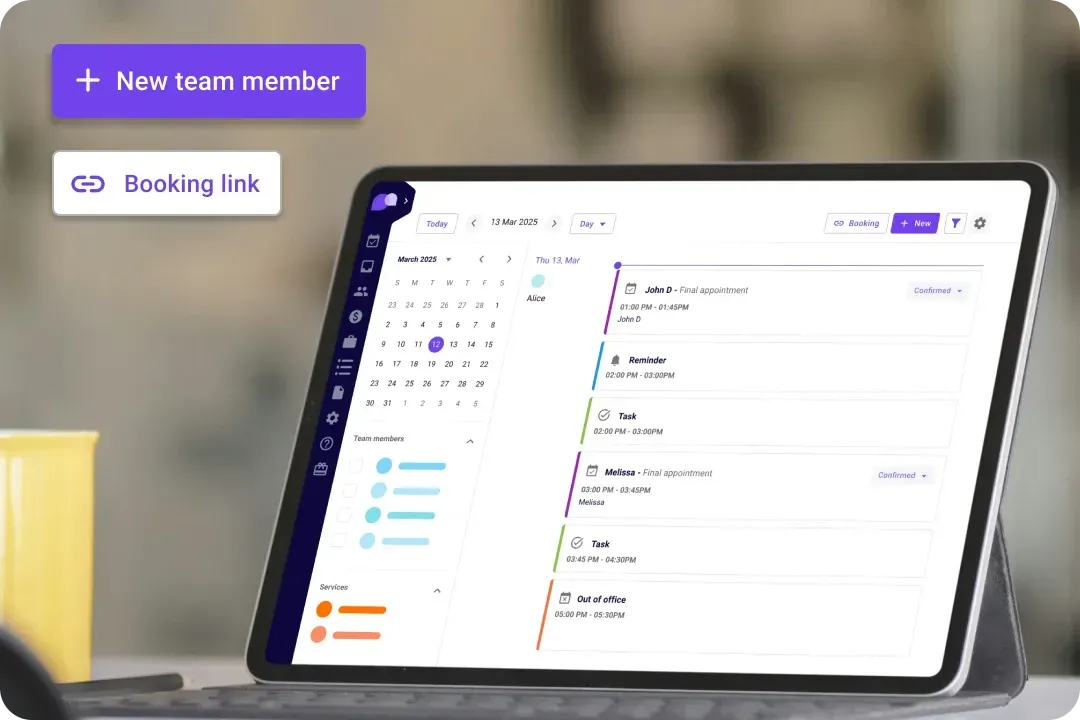
Versatile for all healthcare roles
Carepatron’s billing software solution is designed to be adaptable, supporting a wide range of healthcare services and professionals with ease.

Customizable to various service offerings
Whatever your healthcare practice specializes in, our billing solution can be customized to accommodate your specific service offerings, ensuring seamless financial management.

Tailored to meet diverse financial management needs
Recognizing the unique financial challenges faced by different healthcare practices, our software is tailored to meet these diverse needs, providing a comprehensive solution.

Designed to integrate seamlessly
Our billing software is engineered to integrate smoothly into any healthcare practice, enhancing existing workflows and improving financial operations without disruption.
The benefits of using this free medical billing software
Transform your practice's financial management with Carepatron. Our online medical billing software delivers key benefits that streamline operations, enhance accuracy, and improve your bottom line. Here’s how:

Accuracy
Elevate your practice's revenue with our software that significantly diminishes billing errors, ensuring that financial records are precise and reliable.

Cash flow improvement
Speed up all your billing-to-payment cycles with our practice management software, enhancing your practice's liquidity and financial stability.

Patient-centric focus
By minimizing administrative burdens, our billing software allows your healthcare team to devote more time and resources to providing high-quality patient care, improving patient satisfaction and outcomes.
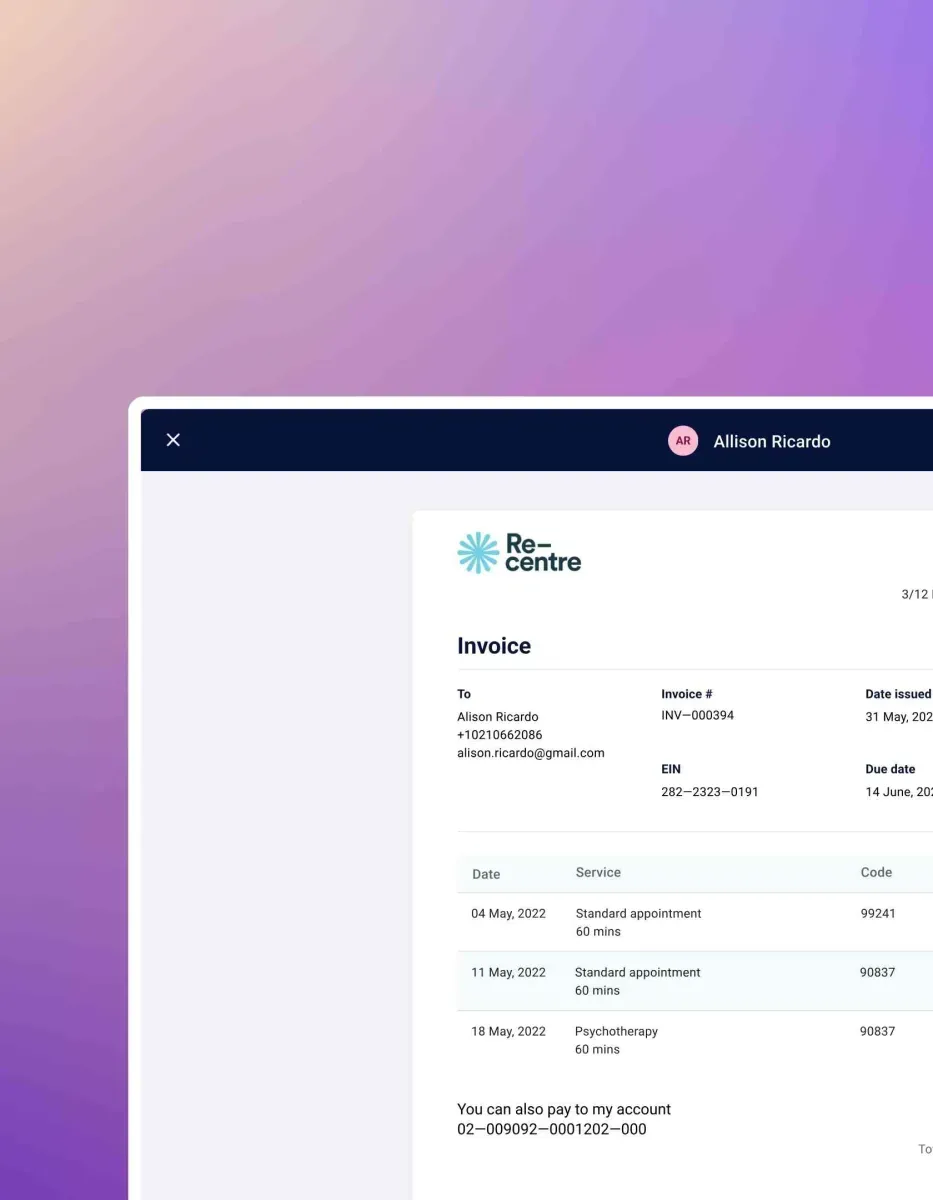
How to use our medical billing software
Integrate Carepatron into your practice and start benefiting from our medical billing software. Follow these straightforward steps for a smoother financial operation:

Quick signup
Begin by easily creating your account, offering a hassle-free start to integrating our billing solution into your practice, free of charge.

Customization
Input your specific service and rate details to customize the system, tailoring it to meet your practice’s unique billing needs and requirements.

Billing
Simplify your billing process with our software, managing invoice generation, claim submissions, and payment tracking, ensuring that your financial operations are efficient and accurate.

Dedicated support
Benefit from our dedicated support team and resource center, providing assistance and tips to help you maximize the use of our medical billing software, enhancing your practice's financial management and overall efficiency.
Frequently asked questions
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments