AI-powered Clinical Documentation
Carepatron brings you cutting-edge clinical documentation software designed to simplify your healthcare practice. Our tool is here to transform how you manage patient records, making healthcare documentation seamless, secure, and efficient. Say goodbye to the hassle of paperwork and welcome a new era of digital health records.
The patient documentation software for your healthcare team
Your team deserves a documentation improvement software that's as dedicated as you are. Carepatron is here to make your days smoother and let you focus where it matters most: on your patients. Here’s why we’re the friendliest choice for healthcare teams:

24/7 support
Our stellar support squad is here round-the-clock, every day of the week, ready to help you with any queries or concerns. Your satisfaction is our top priority as we strive to deliver an exceptional user experience.

Access anytime
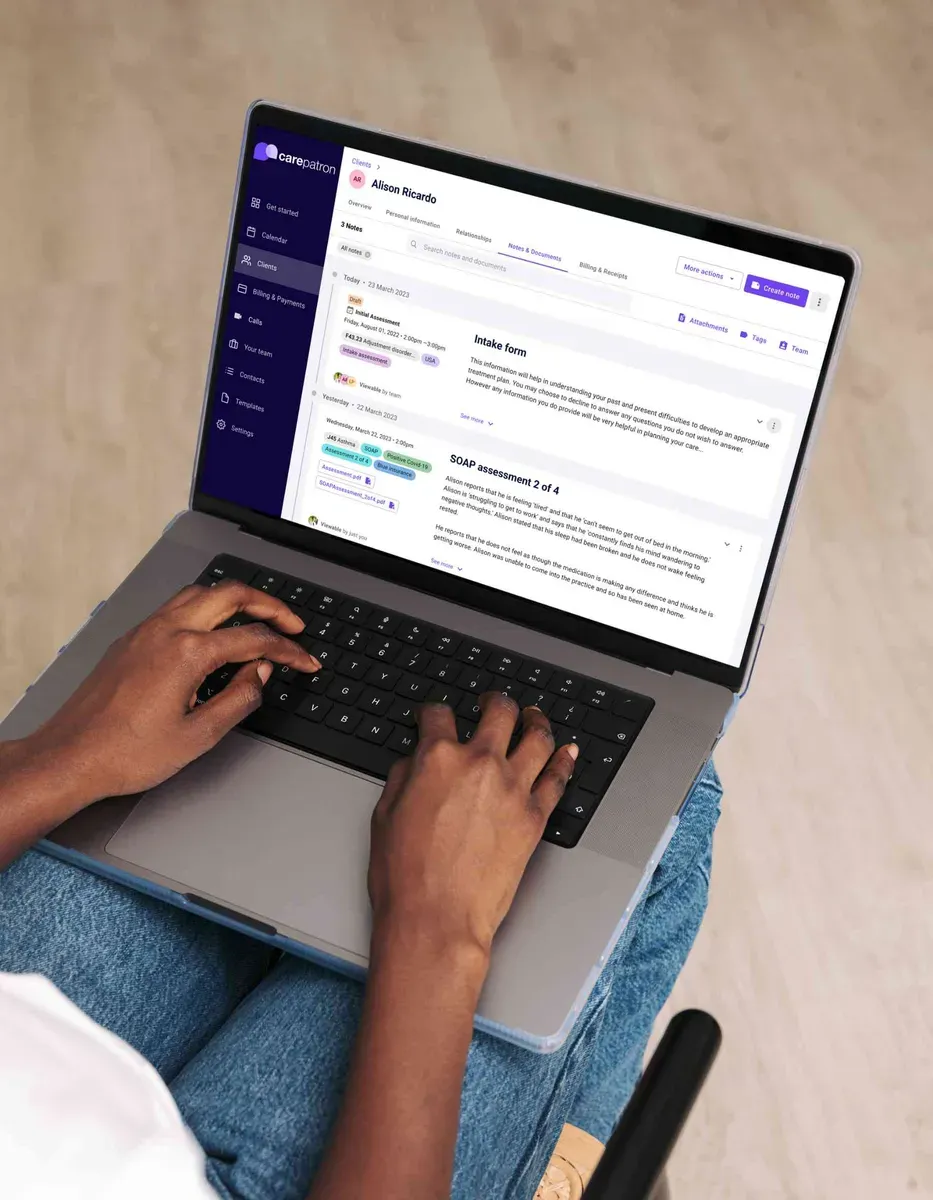
Whether via desktop or mobile, you can access our software anytime, anywhere. Never miss a beat, and stay on top of patient care with our user-friendly interface.

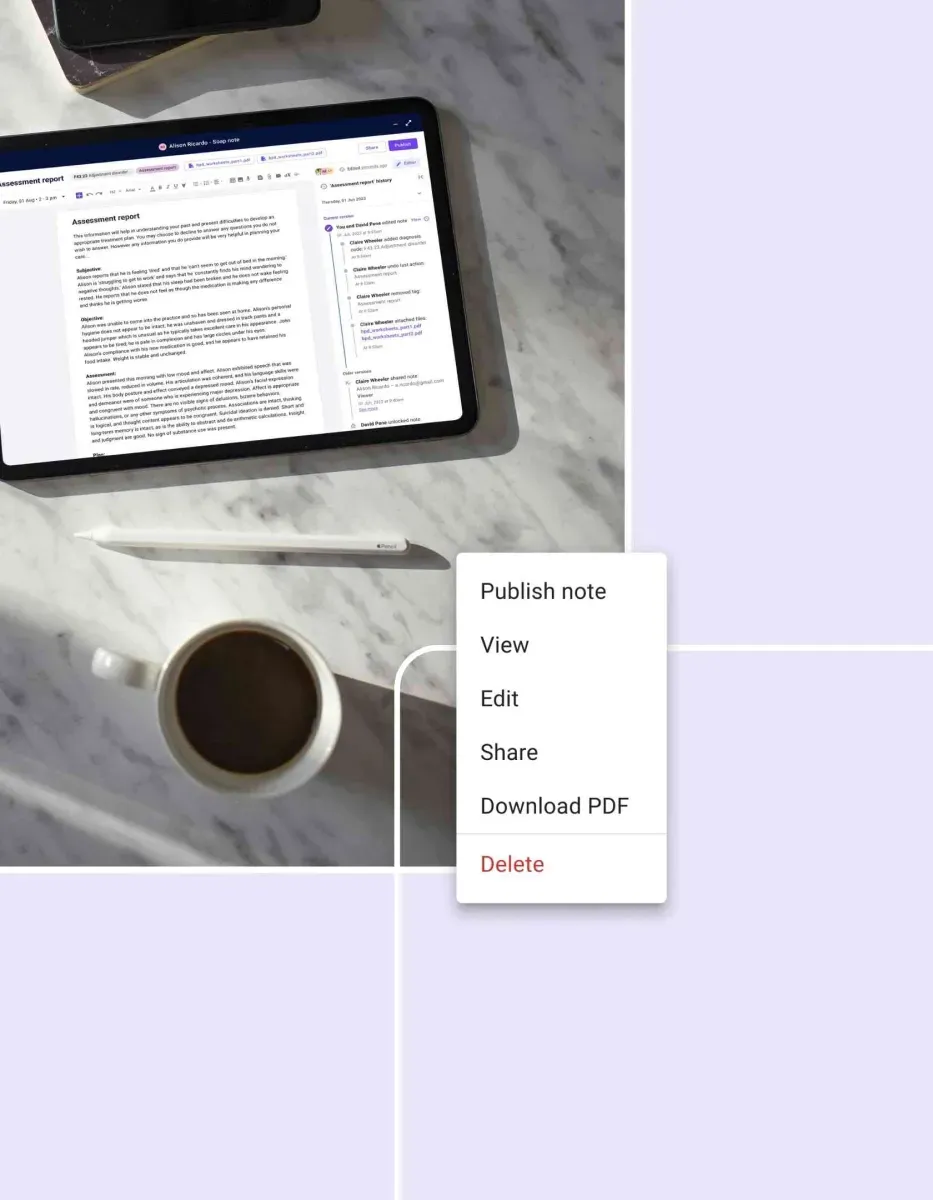
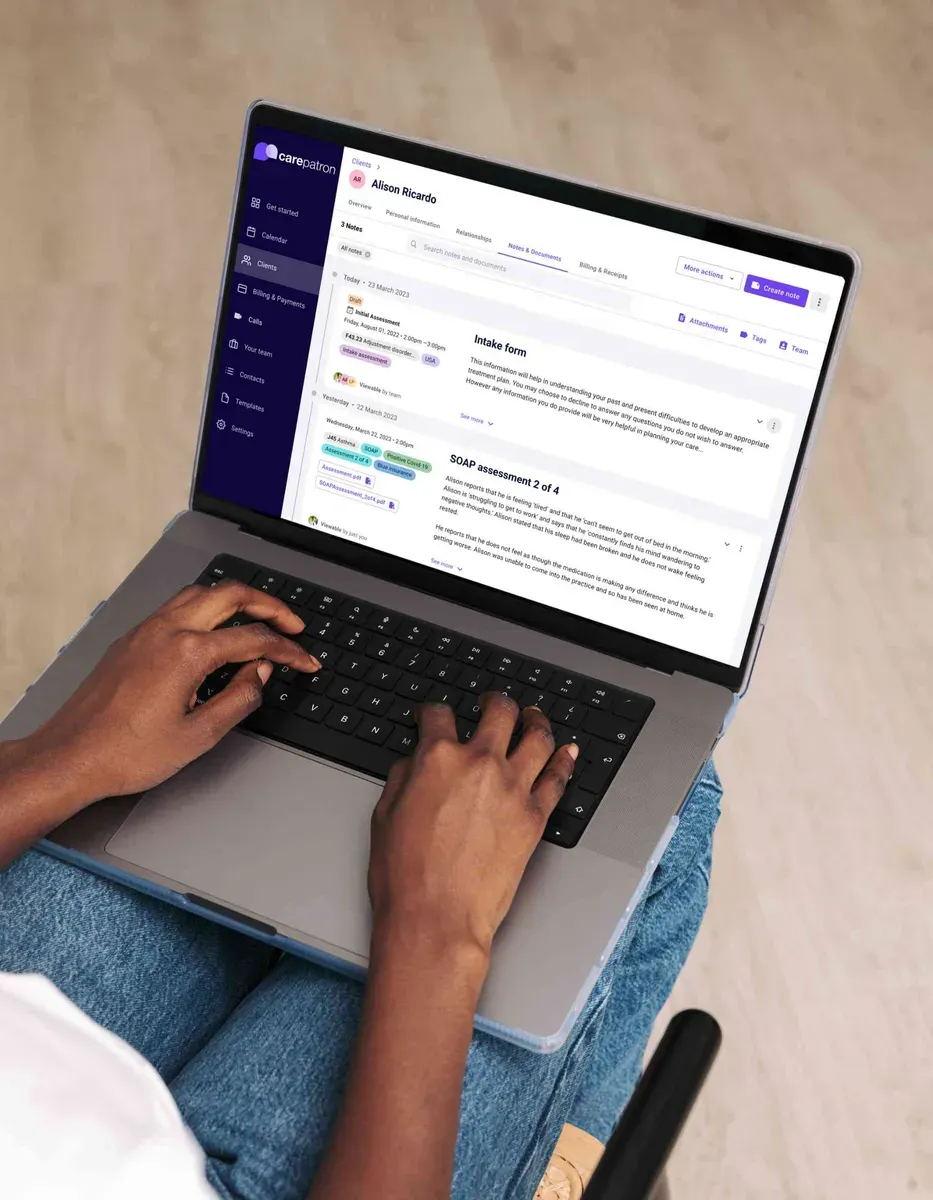
Centralized document management
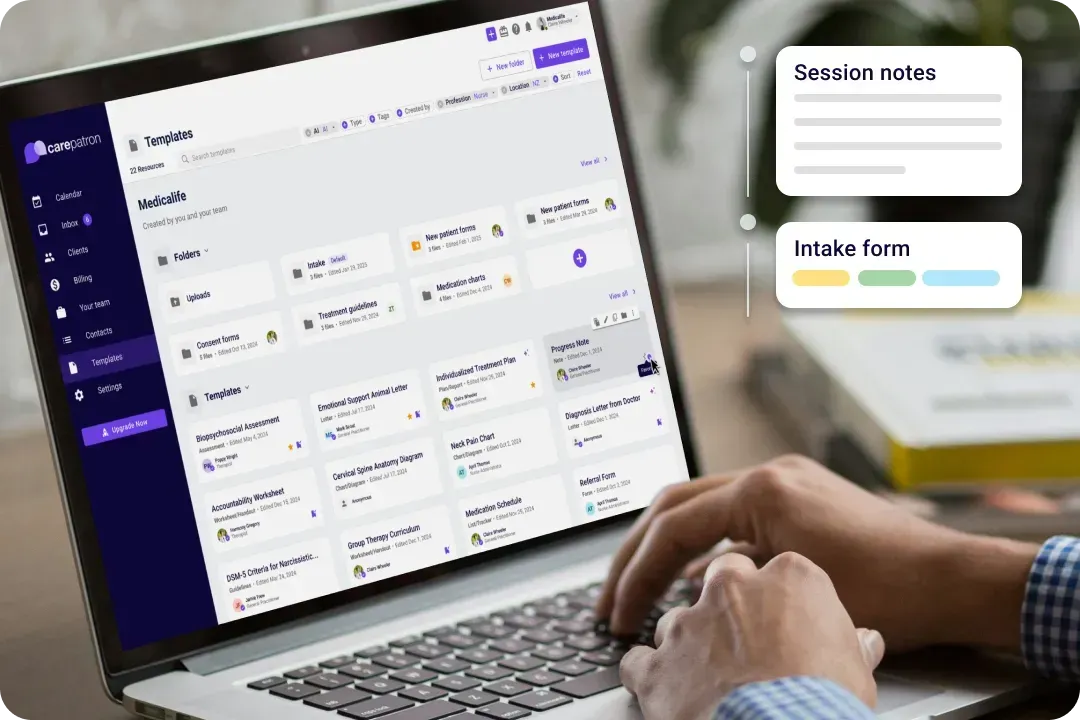
Keep all your team's documents in one place with our secure mental health EHR software, making it simple to find, share, and collaborate on patient files.

Saves time
Streamline your practice with our software, significantly reducing paperwork. This efficiency allows your team to devote more of their valuable time to what truly matters: caring for patients.
Carepatron’s clinical documentation software features
Carepatron brings the warmth of care into the healthcare documentation software with features designed just for the healthcare world. Our tools make clinical documentation thorough and compliant, and a breeze to manage. Here’s what sets us apart:

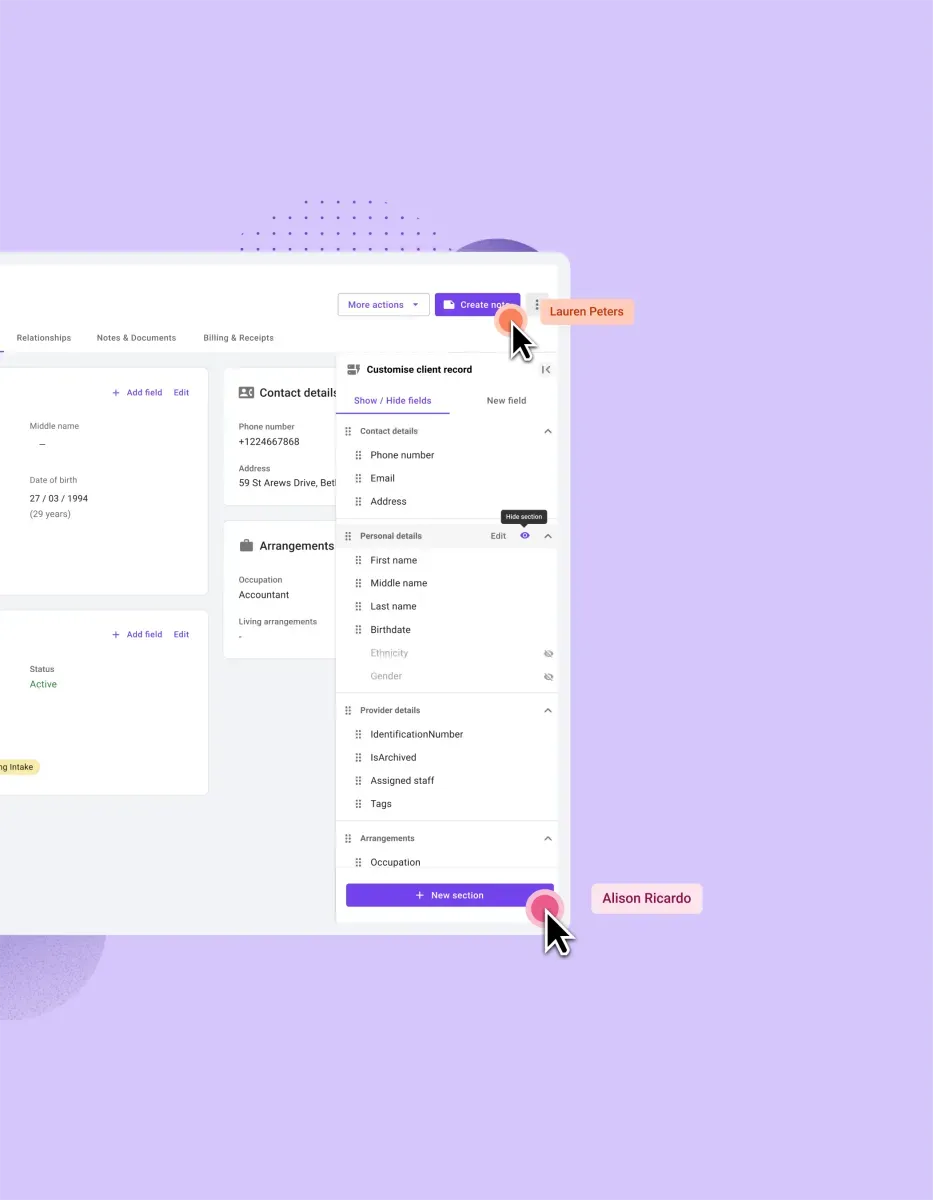
Keeps things accurate
Ensure the accuracy of your records with our system. By minimizing errors and enhancing information flow, we keep your entire team well-informed and aligned, enhancing patient care quality.

Easy access
Gain anytime, anywhere access to patient information. Our platform enhances connectivity and control, ensuring critical patient data is always within reach, thus facilitating better decision-making and patient management.

Works with you
Seamlessly integrate our software into your current operations. We design our solutions to complement your workflow, making the transition smooth and maintaining continuity in patient care without any disruptions.

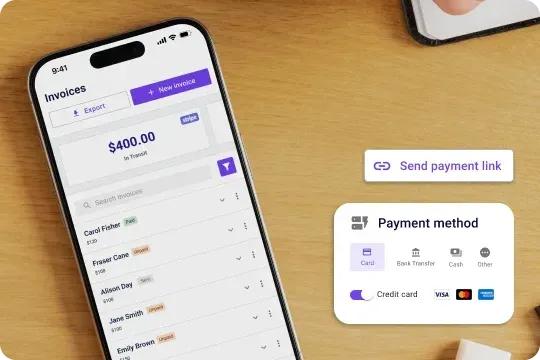
Payment processing in seconds
With our general practice billing software's integrated payment processor, you can easily accept payments from patients and insurance companies. No more waiting for checks to clear or manually processing credit card payments.
Trusted by more than 100,000 practitioners

"It’s so easy to connect with my staff"
CLAIRE, PHYSICAL THERAPIST

"Carepatron saves me 2 hours everyday"
AEGEUS L, HEALTH COACH

"My team loves how simple it is to use"
ANDREA MAGNUS, PRACTICE MANAGER

Clinical documentation software for all healthcare teams
No matter your role in the healthcare journey, Carepatron is your sidekick, ready to support you with versatile tools that adapt to various healthcare fields. Here’s how we help everyone from solo practitioners to large teams:

Unmatched support and community
Carepatron has become the best solution by providing unparalleled support and fostering a vibrant community. Coaches can rely on a dedicated support team and connect with peers for insights, creating a collaborative environment for success.

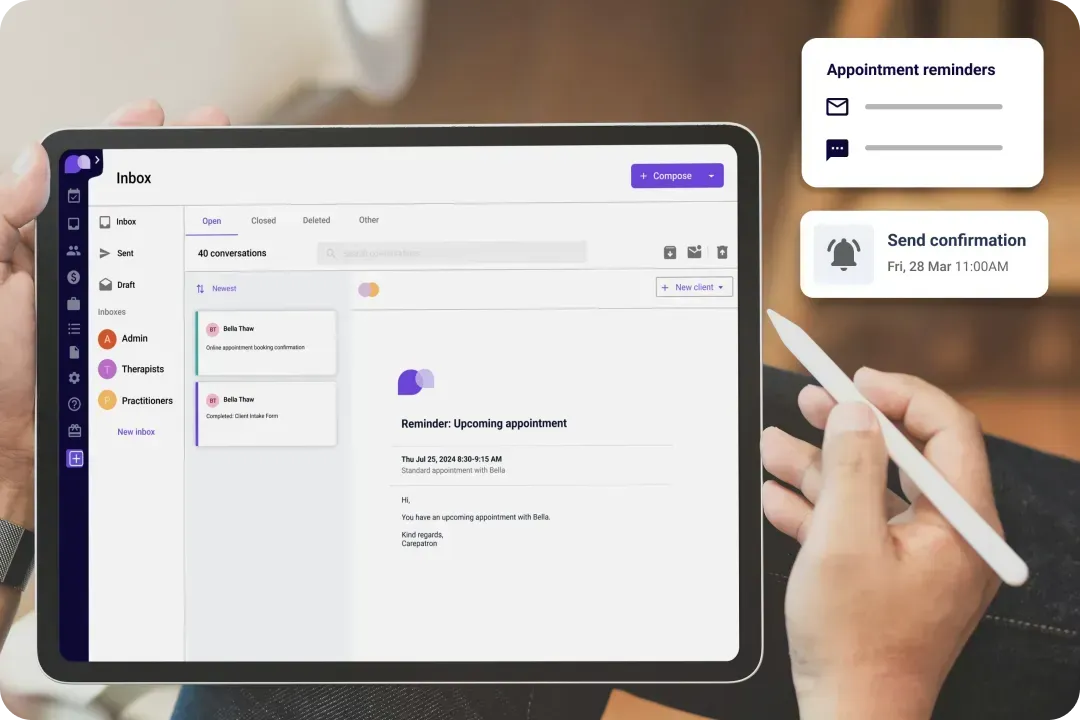
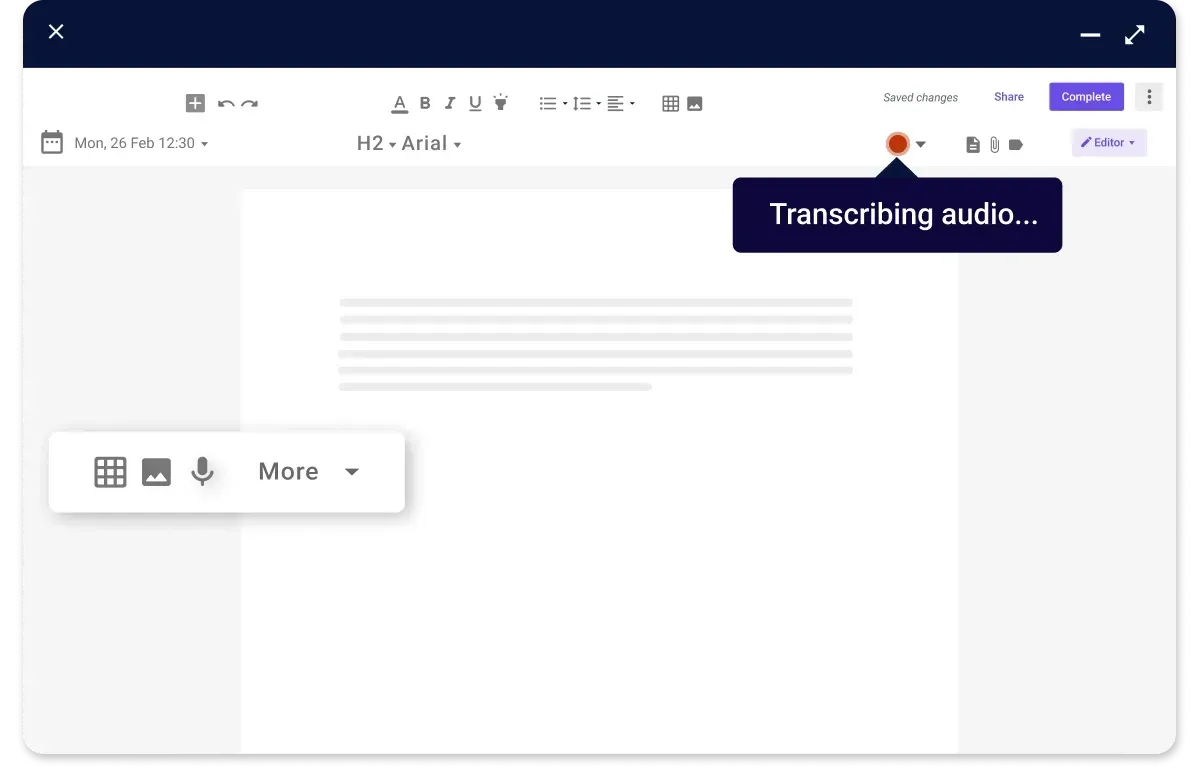
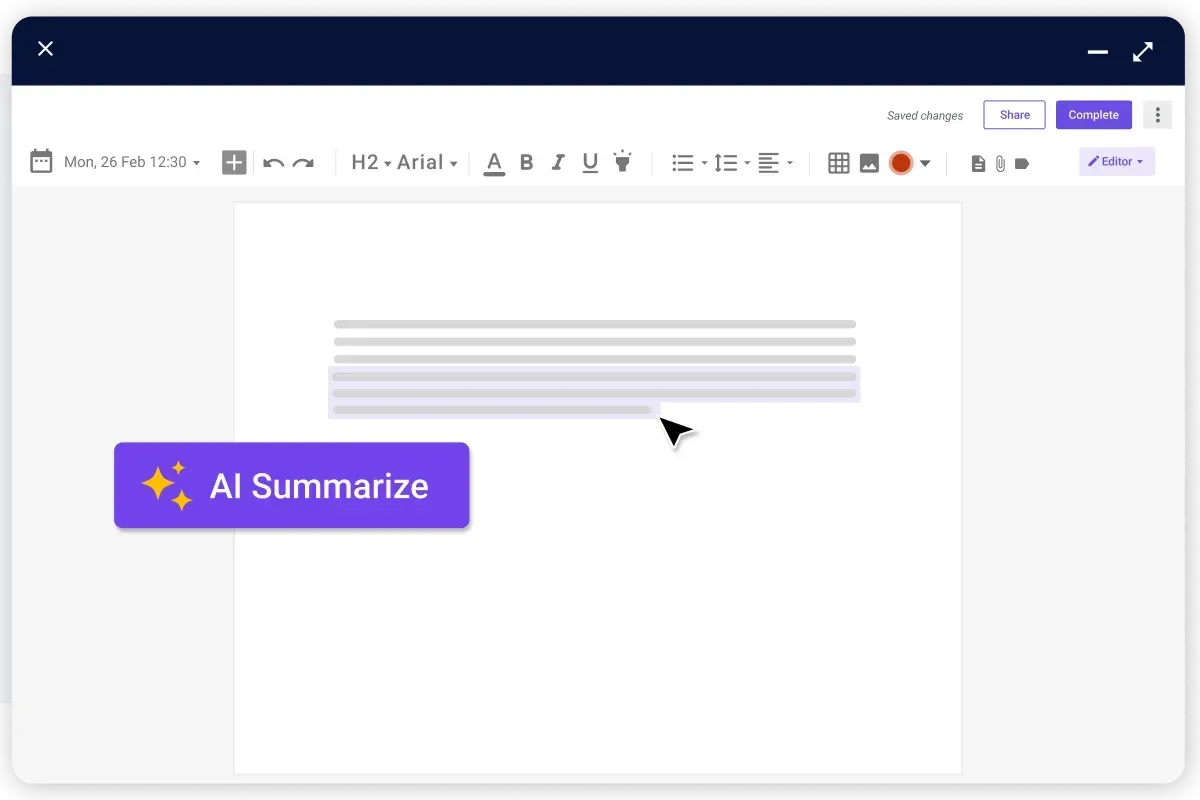
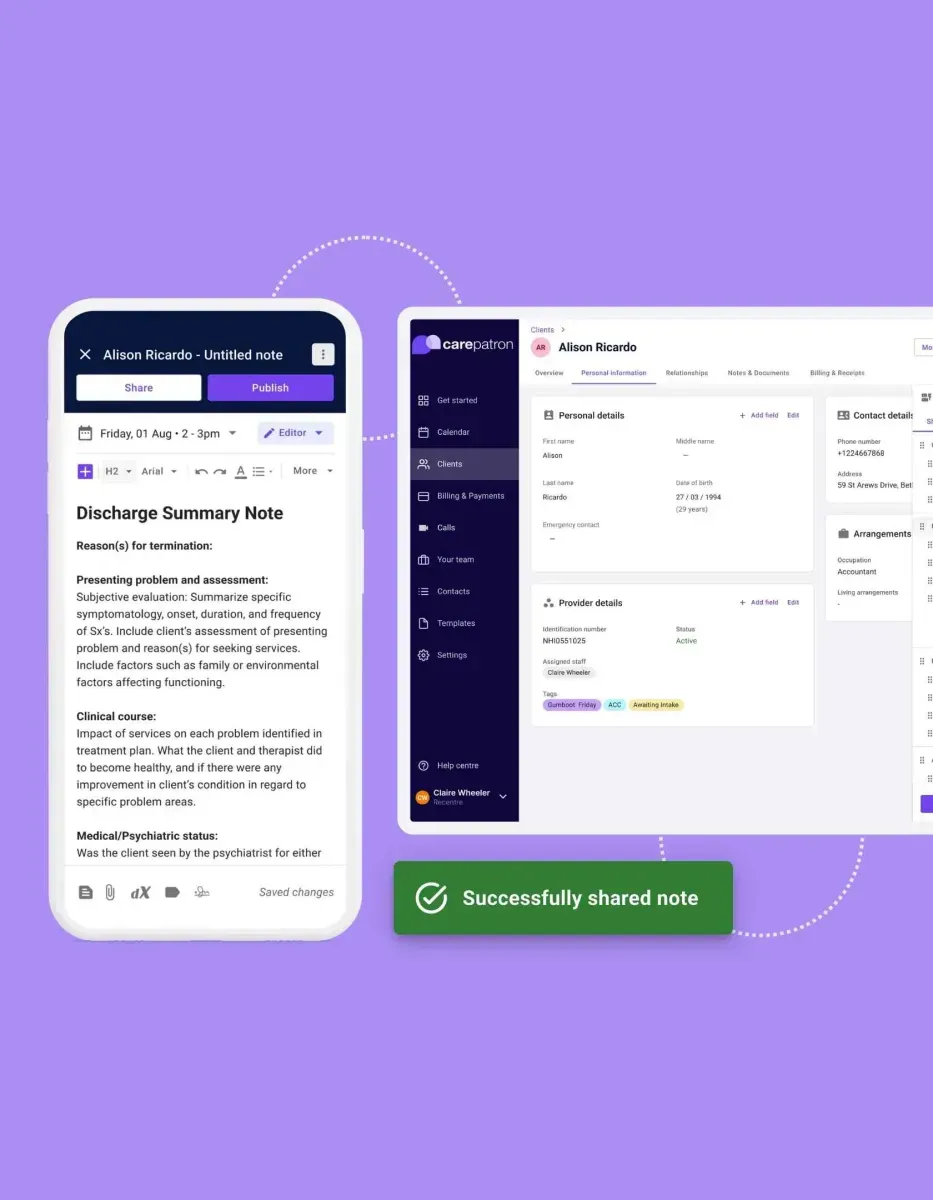
Automatic notes
Our software revolutionizes patient interaction with its quick note-taking feature, enabling healthcare providers to engage effectively with patients. This efficiency enhances patient care quality, fosters better communication, and ensures no details are missed.

Safe and secure
Prioritizing patient confidentiality, our platform employs advanced security measures to safeguard patient details. With end-to-end encryption and compliance with healthcare regulations, we ensure that all patient information remains confidential and secure.
The benefits of Carepatron’s clinical documentation improvement software
With Carepatron, you gain more than just software — you gain a partner in clinical excellence. Our documentation improvement software offers numerous benefits:

Tailor-made templates
Adaptability is key in healthcare, and our software offers customizable templates to suit your practice's needs. Whether it's adapting forms for specific treatments or streamlining documentation processes, our templates allow for a personalized approach.

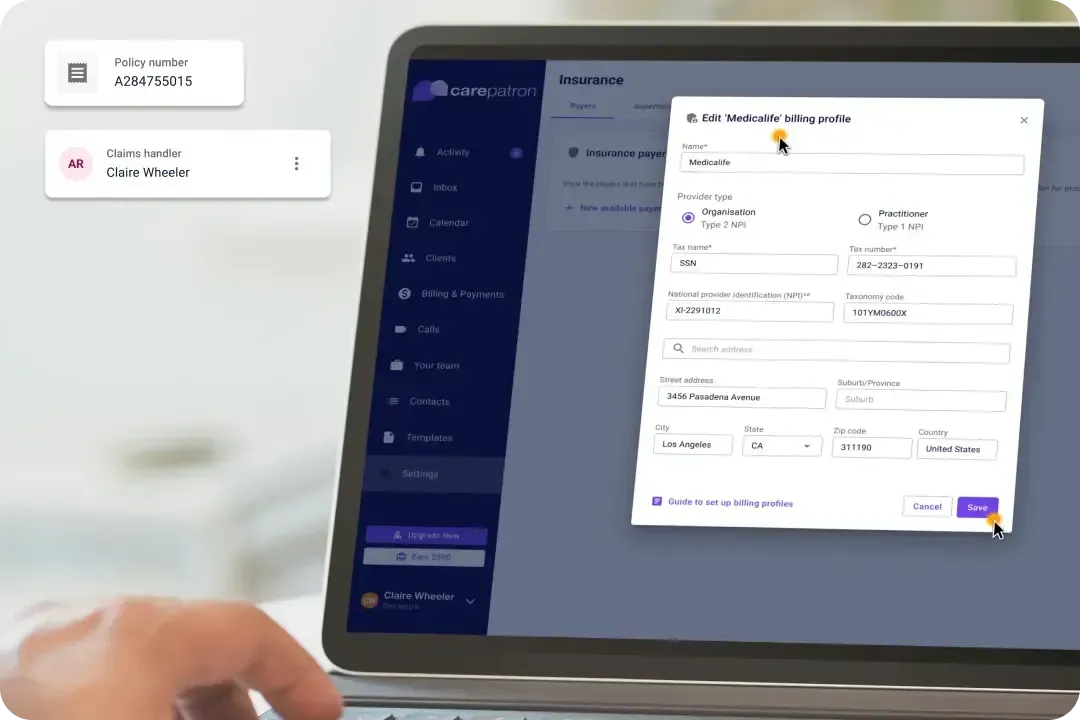
Straightforward billing
Our billing system simplifies the financial aspects of healthcare management. By streamlining billing processes and reducing administrative burdens, healthcare providers can focus more on patient care.

Nurses
Nurses can expedite note-taking processes, ensuring timely and accurate documentation of patient assessments, interventions, and responses for better care coordination.
How to use our free clinical documentation software
Carepatron opens doors to a more organized, efficient practice without costing a dime. Our hospital documentation software, clinical tools, and other resources are designed with your needs, from sign-up to daily use, ensuring you get the most out of every feature. Here’s how to get started and make the most of Carepatron:

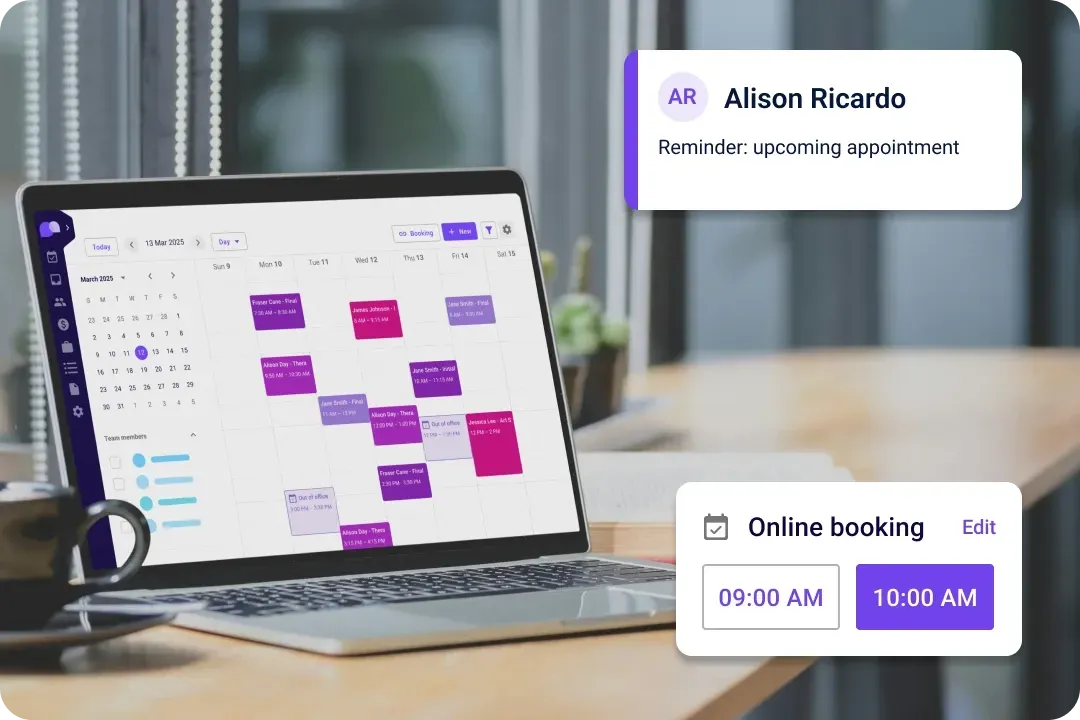
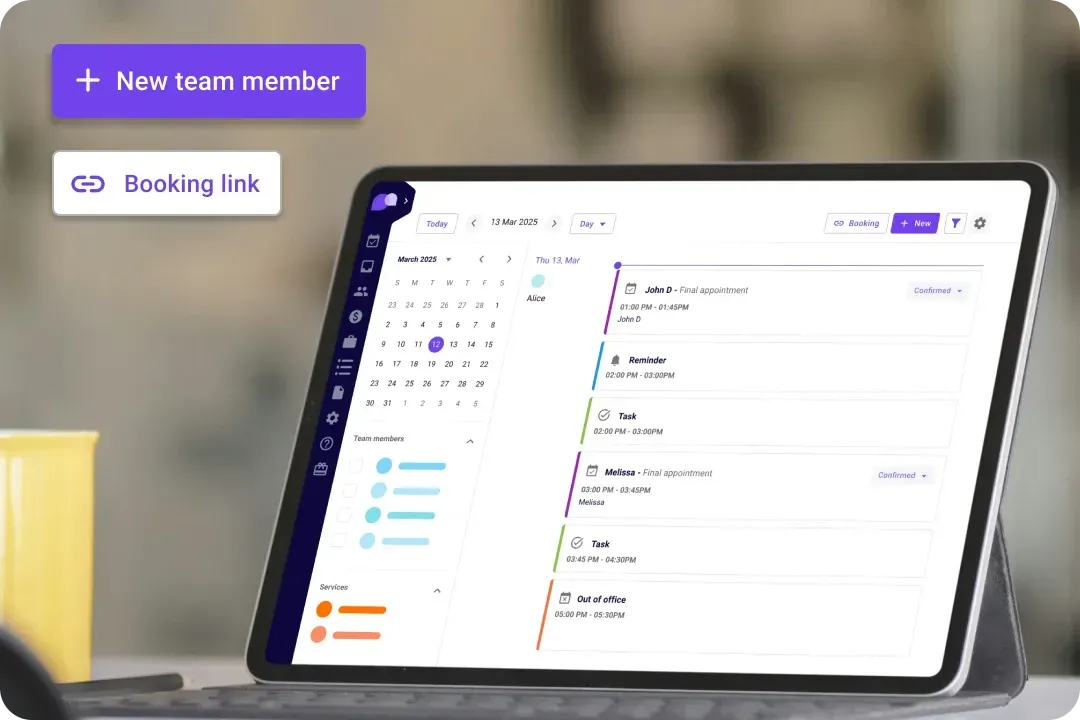
General practitioners
Designed to keep GP practices running smoothly, our software integrates patient records, appointment scheduling, and billing into one seamless system. This approach ensures efficiency and organization, allowing GPs to focus on patient care.

Mental health experts
Recognizing the sensitive nature of mental health care, our platform offers features that ensure confidentiality and security. By facilitating worry-free patient management, mental health professionals can focus on providing compassionate care.

Upgrade for your needs
Want even more advanced features? Upgrade to our professional or organization plan and unlock additional tools for your mental health practice. Choose the best plan for your needs and grow your practice with Carepatron.

Efficient task management
Effortlessly distribute tasks among your team members utilizing our advanced physical therapy scheduling software. Stay organized and enhance collaboration by ensuring everyone is informed with real-time updates and seamless communication.

Total control with telehealth
You and your patients can access appointments, consultations, and follow-ups from anywhere in the world. Our telehealth feature offers secure video conferencing and messaging for reliable virtual care.
Frequently asked questions
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments