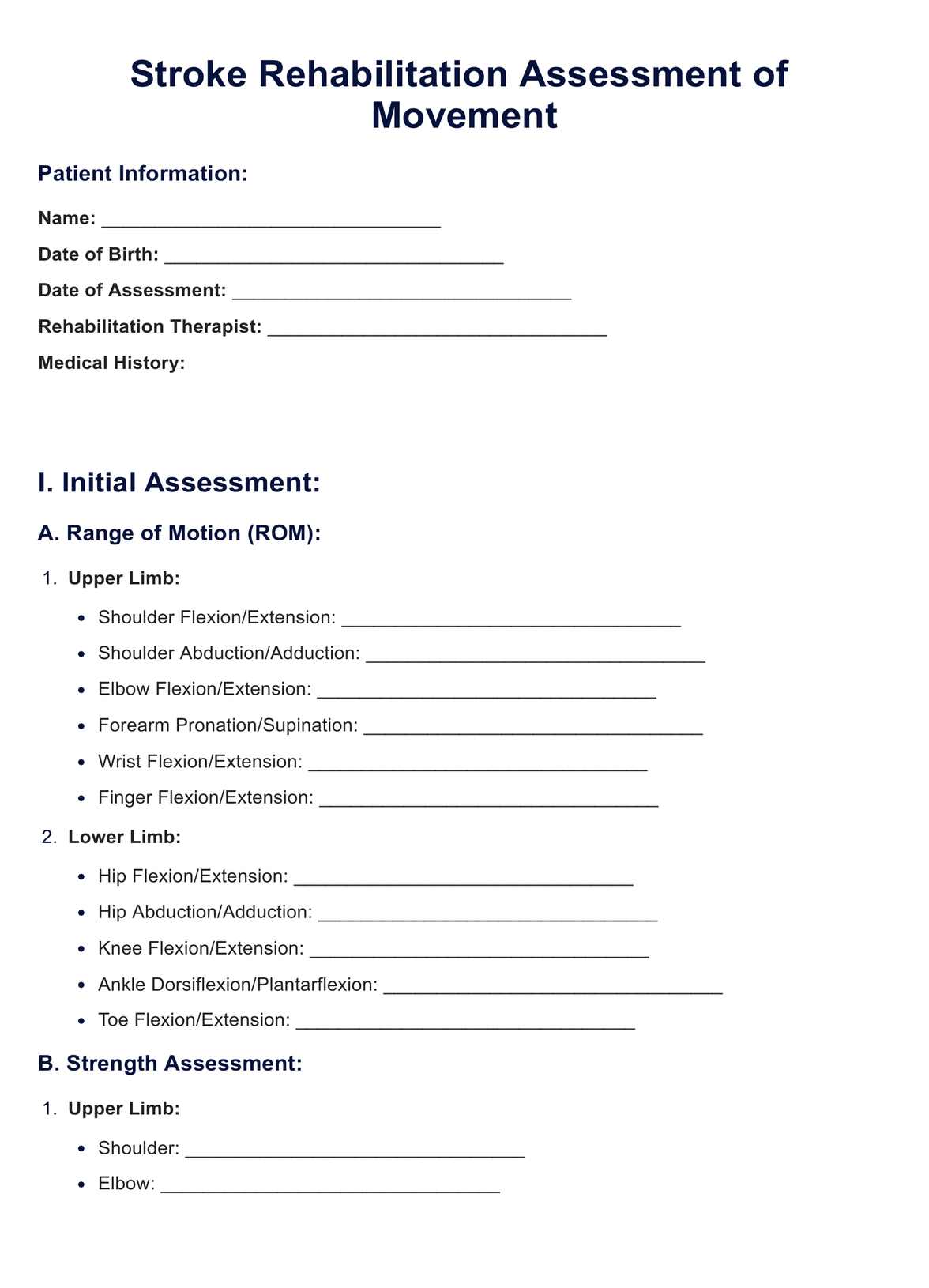
The Stroke Rehabilitation Assessment of Movement systematically evaluates motor abilities and functional movement patterns in individuals recovering from a stroke. It involves standardized tests and measures to quantify impairments, guiding the development of personalized rehabilitation plans.
The Stroke Rehabilitation Assessment of Movement (STREAM)
Looking for a stroke rehabilitation assessment of movement? Download a free PDF from Carepatron and effectively assess movement in stroke patients.
The Stroke Rehabilitation Assessment of Movement (STREAM) Template
Commonly asked questions
The physical assessment for a stroke patient involves evaluating muscle strength, range of motion, balance, and coordination. Physical therapists use this assessment to identify specific impairments and design targeted interventions to improve overall motor function.
The Stream Assessment aims to provide a streamlined and comprehensive evaluation of stroke patients' functional abilities. It focuses on key outcome measures, facilitating efficient data collection and contributing to developing personalized rehabilitation plans.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











