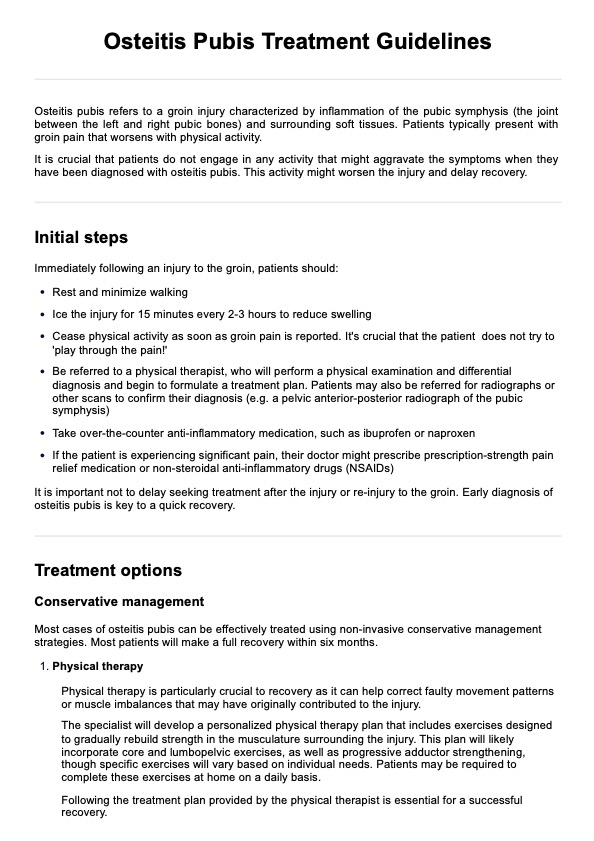
Osteitis pubis refers to a groin injury characterized by inflammation of the pubic symphysis (the joint between the left and right pubic bones) and surrounding soft tissues.
Osteitis Pubis Treatment Guidelines Handout
Access our handy guidelines for effectively treating osteitis pubis. Read more!
Osteitis Pubis Treatment Guidelines Handout Template
Commonly asked questions
Symptoms vary, but patients typically present with groin pain that worsens with physical activity. They may experience hip pain, inner thigh pain, and difficulty walking normally, as well as swelling of the groin area.
Osteitis pubis can be difficult to diagnose as its symptoms often mirror those of adductor tendinopathy or a pulled muscle in the groin. A physical exam, in which an examiner will palpitate the pubic bone to detect pain, is the first step in diagnosing osteitis pubis. Scanning the pubic symphysis with a pelvic anterior-posterior radiograph can be useful to confirm osteitis pubis diagnoses.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments










