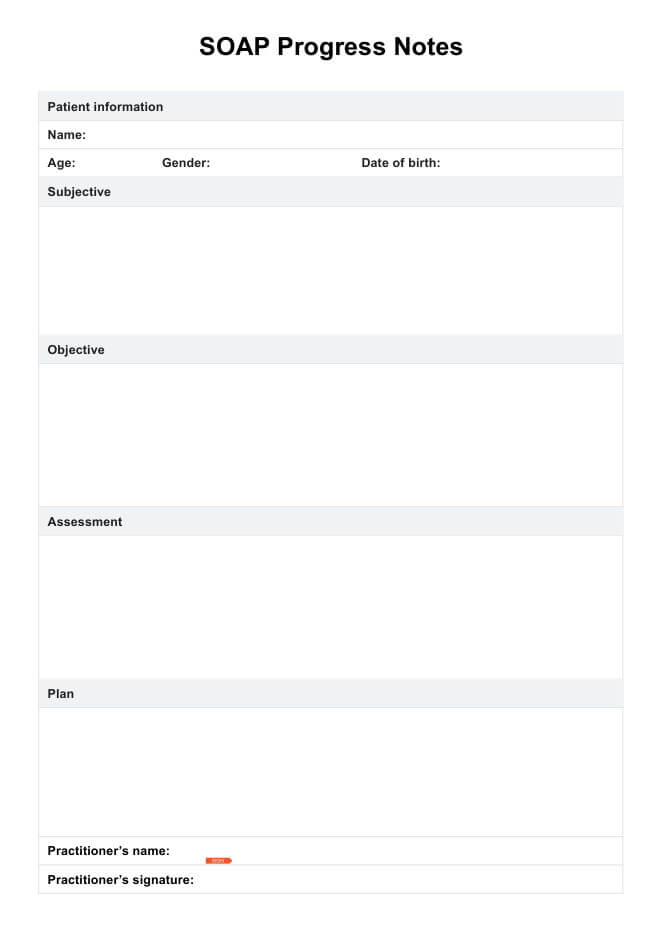
A SOAP progress note is a structured method for documenting patient encounters in healthcare settings. It organizes information into four sections: Subjective, Objective, Assessment, and Plan. This format helps clinicians record patient progress clearly and consistently while supporting continuity of care.
SOAP Progress Notes Template
Enhance clinical accuracy and save valuable time with our SOAP Progress Notes Template.
SOAP Progress Notes Template Template
Commonly asked questions
Start with the Subjective section, summarizing the patient’s reported symptoms or concerns. Follow with Objective findings, such as vital signs or test results, then add your Assessment of the situation and diagnosis. Conclude with a Plan outlining treatment steps, follow-ups, or referrals.
Yes, a SOAP note is a type of progress note commonly used in healthcare documentation. It provides a standardized framework for tracking patient care and clinical reasoning over time. SOAP notes ensure that every encounter is recorded systematically for better communication and accountability.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











